Natural pain relief
Whether you’re still at
home and it’s too early in labor to get pain medication, or you’re
trying to wait it out at the hospital to see if you really need drugs,
you can try any or all of the following techniques that may help to
relieve pain without medication:
Aspirin: not for labor pain
When you start to experience the pain of labor contractions
at home, no matter how tempting it may be, do not reach for an aspirin
to relieve your pain. Aspirin can be extremely dangerous during
pregnancy, particularly in the third trimester and leading up to labor
and delivery. The drug interferes with your blood-clotting ability,
which means that your risk of a hemorrhage during delivery increases if
you take aspirin in the weeks leading up to your baby’s birth. Taking
too much aspirin in the last trimester may actually prolong labor.
Bleeding problems may even develop in your newborn. Taking aspirin
regularly toward the end of your pregnancy can also affect your baby’s
heart or blood flow, so it’s best to avoid aspirin, unless your doctor
recommends you take it. Your best bet for dealing with labor pain at
home is to keep active until it’s time to head to the hospital. While
you wait, do something to distract yourself from the pain, whether it’s
counting the length of time between contractions, packing your bag for
the hospital or anything else that feels right. Ask your partner for a
massage or try a warm shower. No matter what you do, refrain from drug
use. This way, if you need pain relief when you get to the hospital—many
women do—you won’t have any medication in your system.
Opioids
Advantages
Opioids help you to relax during labor, which can help you to conserve your energy between contractions.
Opioids can produce a feeling of well-being, which many women find beneficial during labor.
Disadvantages
Many
women report feeling nauseous with opioids, which can be an unexpected
and unpleasant side effect on top of your pain and contractions.
Opioids can cause dizziness, and this can be can be disorientating during labor.
Some
women have reported feeling out of control with some opioid medications
and therefore out of touch with how their labor is progressing.
Opioids
cross the placenta easily and pass into the baby’s bloodstream. This
can have the affect of sedating the baby and can affect the baby’s
breathing after the delivery. The administration of opioid medications
therefore needs to be carefully timed during labor so that they are not
given too close to the time of the delivery of the baby.
Opioids
can depress the mother’s breathing during labor. However, this side
effect is more common when the mother has a preexisting respiratory
illness, such as asthma or emphysema.
Opioids
cause a delay in emptying the bowels and therefore increase the overall
risk to the mother should general anesthesia be needed later on (see General anesthesia).
Opioids (pethidine and diamorphine)
Advantages
Opioids help you to relax during labor, which can help you to conserve your energy between contractions.
Opioids
can be administered by a doctor or a midwife. A doctor can give an
advance prescription at around 36 weeks so that an opioid can be given
by a midwife at a home birth.
Diamorphine produces a feeling of wellbeing, which many women find beneficial during labor.
Disadvantages
Many women report feeling nauseous with opioids. Pethidine in particular has side effects of nausea and vomiting.
Opioids can cause dizziness, which can be disorientating during labor.
Some women report feeling out of control with pethidine and therefore out of touch with how their labor is progressing.
Opioids
cross the placenta easily and pass into the baby’s bloodstream. This
can have the effect of sedating the baby and can affect the baby’s
breathing after the delivery. The administration of these drugs
therefore needs to be carefully timed during labor so that they are not
given too near the time of the delivery of the baby.
Opioids
can depress the mother’s breathing during labor. However, this side
effect is more common when the mother has a pre-existing respiratory
illness, such as asthma or emphysema.
Opioids
cause a delay in emptying the bowels; if general anesthesia is needed
later, this increases the small risk of stomach contents being inhaled
into the lungs under anesthesia.
Considering an epidural
Pros
An
epidural provides absolute pain relief in 90 percent of cases; 10
percent of women have some degree of residual pain, but still have a
marked improvement in their overall discomfort.
Epidurals do not pose any risk to your baby.
The
presence of an effective epidural means that if intervention is needed
at any time, the epidural can be topped off with anesthetic for either
an assisted delivery with forceps or vacuum, or a cesarean delivery.
This also reduces the likelihood that a general anesthetic will be
needed.
Cons
Around 1 in 10 women do not experience absolute pain relief with an epidural.
Some women develop a headache that persists after an epidural (see An Epidural “headache”).
A rare complication is patches of heaviness in the legs or feet.
There are a few very rare risks with an epidural
In
common with all invasive procedures, inserting an epidural can result
in infection. Meningitis occurs in around 1 in 100,000 women and an
epidural abscess occurs in about 1 in 50,000 women.
There is a 1 in 170,000 risk of developing a blood clot in the epidural space (epidural hematoma).
There
is a 1 in 100,000 risk of the epidural tube moving into the fluid
around the spine and resulting in unconsciousness, and there is a 1 in
250,000 chance of the epidural causing some form of paralysis.
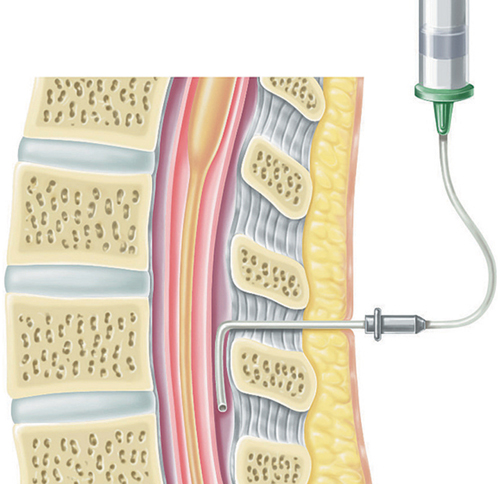
How an epidural is done
If you opt for an epidural, the doctor should explain the procedure to you, and you should have the opportunity to ask the anesthesiologist any questions.
Getting ready for an epidural
Before starting the
epidural, a plastic tube will be placed in a vein in the back of your
hand or in your arm, to which an IV containing fluid will be connected.
You are given fluids during an epidural to stop your blood pressure from
dropping. The doctor will then help you into the correct position to
receive the epidural, which will either be sitting up with your legs
over the side of the bed leaning forward, or curled up on your side on
the edge of the bed. The position may depend on the preference of the
anesthesiologist.
Your lower back will
be cleaned with antiseptic and a drape placed over the rest of your back
to reduce the risk of infection. Before the epidural needle is
inserted, a local anesthetic will be given into the skin and surrounding
tissues. This creates a numb patch to ensure that the insertion of the
large epidural needle is not painful. When the local anesthetic is
injected, you may feel a scratching sensation and experience a very
short-lived sting in the area between the vertebrae bones
The procedure
Since it’s important for
you to remain still during the procedure, the anesthesiologist will
insert the epidural between your contractions. If this is difficult, you
should try to concentrate on your breathing and remain as still as
possible until the procedure is completed. You will feel a pushing
sensation in your back while the anesthesiologist is trying to find the
very small epidural space with the hollow needle. When the space is
located, a tiny plastic tube will be fed into it through the needle. The
epidural needle is then removed and the tube, which is secured onto
your back with sticky tape, remains in the epidural space. The tube
remains in place until your baby is delivered and, because it is very
thin, soft, and pliable, it is perfectly safe to lie on the tube and to
move around.
Managing the epidural
Once the epidural tube
is successfully in place, the anesthesiologist will give the first dose
of medication through it by means of a syringe. Once she is satisfied
that the epidural is in the correct position and is working effectively,
all subsequent doses, or “top ups,” can be given without another
injection. Your blood pressure will be taken once the epidural is in
place and will be monitored for the next half an hour or so, and then
regularly thereafter, including after each top up. Each dose of
medication takes around 10–20 minutes to take its full effect and can
last between one and two hours. The epidural will be topped up as
required, usually around every three to four hours, to keep you
comfortable throughout your labor. An anesthesiologist should be
available 24 hours a day to manage any concerns or problems that may
arise with the epidural.
Before the epidural is given,
your back will be covered with a sterile sheet and then a local
anesthetic will be given to numb the area so that you don’t experience
pain when the larger epidural needle is inserted.

The anesthetic is given through a tube that is inserted into the epidural space, avoiding the spinal cord and its covering.
An epidural “headache”
Some women report a headache after an epidural, which can develop more than 24 hours
after the delivery and tends to be at the front of the head. It is made
worse by sitting up and moving around and is much improved by lying
down. This occurs in around 1 in 100 women and is caused by the epidural
needle moving too far forward and cutting the dura sheath, the membrane
maintaining the fluid around the spinal cord and brain. This small hole
results in a loss of fluid from the sheath, which causes a headache.
The risk is hugely reduced by remaining still during the placement of
the epidural. In around 70 percent of women, the hole heals on its own.
You will be advised to drink plenty of fluids and to take simple
painkillers, such as acetaminophen and ibuprofen and you will be
reviewed at regular intervals by an anesthesiologist.
If the headache
persists, a procedure called a “blood patch” will be done. This is done
in the sterile environment of an operating room by two
anesthesiologists. One places an epidural needle in your back, while the
other takes around 20 ml of blood from a vein in your arm. The blood is
then passed down the needle into the epidural space. This forms a clot
that seals the hole and prevents further leakage of fluid from around
your spine, therefore relieving the headache.
Epidural pain relief
Alice was having her
first baby. Her pregnancy had been uncomplicated and she had written a
birth plan with her husband outlining her desire for a natural
childbirth by keeping active and using TENS and then warm water to deal
with contractions. Alice also stated that she wanted to avoid an
epidural if possible.
Alice’s birth story:
My husband and I
arrived at the delivery suite in early labor. I started to use a TENS
machine for pain relief. However, as my labor progressed, I became very
distressed since I hadn’t anticipated that the contractions would be so
painful. When I was around 3 cm dilated, I decided to remove the TENS
machine and get into the bath. My husband gave me a back massage and
provided emotional support. However, I think he struggled to understand
my discomfort and he needed support from the nurse. After 15 minutes, I
decided to get out of the bath since it was providing little pain
relief. I used a birth ball to stay active and my husband gave me more
massage and acupressure. I coped well for the next hour, but then became
increasingly exhausted and upset. When I was examined, I was only 5 cm
dilated. We both felt despondent because we had hoped I was further
along.
My nurse then suggested
that I talked to the anesthesiologist about my options for further pain
relief, and as a result of my conversation with the anesthesiologist, I
decided to have an epidural. I told the anesthesiologist that I’d had an
epidural a few years ago for knee surgery and how it had provided
excellent pain relief, but that I had itched for hours afterward. The
anesthesiologist surmised that the itch was caused by one of the
painkilling medications (fentanyl) in the epidural top up and agreed
that this medicine wouldn’t be used.
The anesthesiologist agreed
to do a low dose combined spinal epidural that gave absolute pain
relief within five minutes. My legs were a little heavy at first, but
they felt fine within an hour. I felt that we were both able to take
time out after the epidural and that I was able to refocus on my labor. I
felt pleased that I’d managed a large part of my labor without pain
relief, and was happy with the decision to have an epidural when I did. I
had an unassisted delivery later that evening and gave birth to a
beautiful baby girl.
The anesthesiologist comments:
Alice kept an open mind
regarding pain relief and understood that different methods of pain
relief could be used at different times during labor. After the
epidural, she no longer felt that her labor was an endurance test and
was able to focus again on her labor and on delivering a healthy baby.
A low dose “mobile” epidural means that you maintain some feeling in your legs and can remain active during labor.
