The growing trend for wheat- free and
dairy-free foods is fuelling a debate about the true nature of allergies and
food intolerances - and their link with weight. But there’s a world of
difference between the two, as we report
Many of us know of
someone with a severe peanut allergy, where the mere hint of the food on
someone else’s breath can trigger an alarming, potentially fatal response. And
most of us also know people who claim intolerance to a particular food, such as
milk, wheat or fruit. Allergies are pretty clear-cut to diagnose, but food
intolerances are much harder, with some critics disputing their existence, and a quarter of us dismissing
sufferers as ‘fussy eaters’.

The
truth about food allergy and intolerance
Dr Adrian Morris, principal allergist at
the Surrey Allergy Clinic, says. ‘Intolerances do appear to be increasing, as I
am seeing more and more people in their 20s to 40s with a suspected reaction to
certain foods. Wheat, in particular, has turned into the new pariah. True
allergies, particularly in children, arc on the increase too.’
In reality, food allergies are rare,
affecting two per cent of adults and up to eight per cent of children. But when
it comes to food intolerances (non-allergic hypersensitivity), the figures rise
dramatically - Allergy UK estimates that up to 45 per cent of adults suffer. So
what’s the difference?
Allergy or intolerance?
True food allergies are caused by the
immune system treating a food, such as peanuts, as toxic and creating an
antibody in response to the 'invader'. Immunoglobulin E (IgE) is released into
the blood, causing an almost instant and dramatic reaction. ‘Symptoms can
include swelling, hives and vomiting,' explains dietitian Helen Bond,
spokesperson for the British Dietetic Association. ‘In severe cases, the
allergic reaction can lead to anaphylactic shock, which can cause swelling of
some parts of the body, such as the lips and throat, and can be fatal if an
adrenaline injection isn't given in time.'

Dietitian
Helen Bond, spokesperson for the British Dietetic Association
Sometimes symptoms are not as dramatic,
though still distressing, and may appear hours or even days later. These are
known as non-lgE mediated allergies and involve a different part of the immune
system. They’re still classed as allergies, but are rarely life-threatening.
Classic foods that cause allergies include
cow's milk, hen’s eggs, shellfish, fish, peanuts, some types of fruit, wheat
and soya.
Food intolerances are adverse reactions to
a specific food or food ingredient, and don’t involve the immune system.
Symptoms are often centered on the gut, causing diarrhea, constipation, wind
and stomach cramps, though in some people, headaches, a stuffy nose and aching
joints can also occur. It can take up to 24 hours after eating the food for
symptoms to appear, which makes identification of the culprit extremely
difficult.

Classic
foods that cause allergies include cow's milk, hen’s eggs, shellfish, fish,
peanuts, some types of fruit, wheat and soya.
The list of foods that potentially cause
intolerance in susceptible people is long. In addition to those causing
allergies listed above, Helen Bond adds caffeine. Chocolate, foods that
naturally contain histamine (such as kiwi fruit and some cheeses) or salicylates
(in brazil nuts and some fruit and veg), plus food additives or preservatives
(such as sulphites and monosodium glutamate).
How do you know?
If you, or your child, have a true allergy
you’re probably already aware of it. But it’s important to have a proper
diagnosis. Your GP can arrange a blood test known as RAST,
which checks for the allergy-immune cells (IgE). If
this is positive, you should be referred to a specialist allergy clinic.
Sometimes a skin prick test is used, where several different substances are
applied to the forearm and the reaction to each is measured.
Testing for food intolerance is much
harder. ‘Only two intolerances can be properly tested: lactose and gluten,’
explains Helen Bond. ‘The former is caused by the lack of the enzyme lactase,
which is needed to digest the natural sugar in milk. This is much more common
in people from Asia, South America and Africa. Three tests are used in
diagnosis: a hydrogen breath test, a blood glucose test and a stool acidity
test.
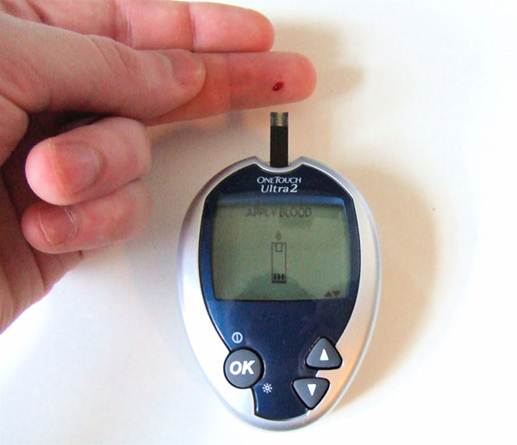
Blood
glucose test
‘Gluten intolerance can indicate coeliac
disease, which is a serious lifelong autoimmune condition of malabsorption of
nutrients, due to damage to the lining of the gut. It’s diagnosed by a blood
test and biopsy of the gut lining.' Undiagnosed, it can lead to problems such
as osteoporosis and bowel cancer. Then there’s gluten sensitivity, which can
cause problems, but isn’t thought to involve the immune system.
The most common test for other food
intolerances involves measuring the immunoglobulin G (IgG) antibody levels in the blood, which are often raised if a
problem with a certain food exists. However, there is continuing controversy
surrounding this, as many experts - Dr Morris among them - believe high levels
of IgG do not indicate a problem, but merely show that some foods naturally
cause high levels of this antibody without any ill effects.
‘As tests for most food intolerances aren’t
available on the NHS,’ explains Dr Morris, ‘this has led to a whole mish-mash
of alternative diagnostic tools in addition to IgG blood tests. These include
vega (electrodermal testing), hair analysis and kinesiology (pressure applied
to legs or arms to test resistance to foods). But there is no scientific
evidence that these tests are reliable. They are expensive and the advice could
be harmful, as this often involves elimination of foods, which could lead to
nutritional deficiencies.'