A mysterious hormonal condition is
afflicting thousands of Indian women. It’s making them heavier and hirsute and
stealing their health and happiness. Are you a victim?
One evening, around three years back, my
roommate and I were relaxing with a hot cup of tea when, out of the blue, she
remarked. “You seem to have put on a lot of weight lately”. I had barely
recovered from the shock of that bald-faced statement than I realized she
wasn’t done. “You’re becoming hirsute and your acne problem seems to have
worsened”, she said bluntly.
Now although I was somewhat offended by my
BOF’s frankness, I realized I was more worried than upset. Probably because I
realized she was simply echoing what was already playing on my mind. I not only
looked fat, I felt fat; acne mottled my oily face which was already scarred by
earlier attacks (even my neck area hadn’t been spared). And I seemed to have
developed a chronic back pain that sapped my energy.

The
private anguish of PCOS
My friend informed me that she’d gone
through a similar phase some time back and had al so suffered menstrual
irregularities. “It turned out to be a condition called Poly Cystic Ovarian
Syndrome. So go see a doctor, stat”, she urged. I dismissed my roomie’s
misgivings, thinking I was just going through the normal hormonal changes that
any 19-year-old faces. Instead I sought a dermatologist for my acne. But a
month of treatment brought no visible improvement.
And then to my alarm, I realized 2 months
had slid by without any sign of my menses. Maybe my friend is right, after all!
With a sinking heart I went to see a
gynecologist and described my symptoms to her.
I was put through a whole gamut of tests –
ultrasounds of the abdomen, blood work to check for hormonal levels, Follicle
Stimulating Hormone (FSH) and Luteinizing Hormone (LH). Dehydroepiandrosterone
(DHEA) and testosterone, thyroid function for menstrual irregularities and male
pattern hair growth, Glucose Tolerance Test (GTT) for blood sugar level. Even
my cholesterol levels were checked! And then I got my diagnosis – it was indeed
Poly Cystic Ovarian Syndrome (PCOS)!
What Is PCOS?
I started researching my condition and
along the way discovered that scores of other young women were in the same boat
as me – Khyati (19) fashion designing student, Shristi (23) literature student,
Aastha (21) interior designer, and Jayati (24) philosophy student. I learnt
PCOS is a group of symptoms rather than a single condition per se. In fact,
cysts on the ovaries, the symptoms for which the disorder is named, are not
even necessarily present. The classic signs are obesity (present in 50 to 60
per cent of cases), excessive facial hair growth, and irregular periods.

I
started researching my condition and along the way discovered that scores of
other young women were in the same boat as me
Also common are elevated triglycerides
(undesirable fats in the blood), high LDL, or “bad” cholesterol, and low HDL,
or “good” cholesterol.
The way the disorder manifests itself
varies. Some women have all of the symptoms, while others have very few, which
can make diagnosis somewhat tricky.
Many of the symptoms of PCOS are
thought to be the result of excess levels of the hormone Insulin
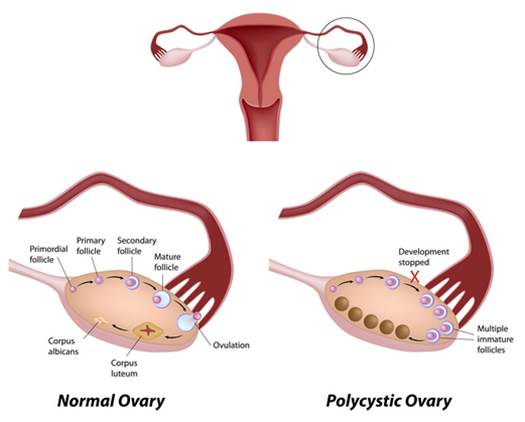
In many women who have the disorder the
ovaries are enlarged and feature numerous small cysts along the outer edge of
each ovary. In a normal menstrual cycle, one egg is released from a dominant
follicle (16+mm size) – essentially a cyst that bursts to release the egg. In
PCOS, there is a so-called follicular arrest, i.e., several follicles develops
to a size of 5 to 7 mm, but no further, leading to infrequent or absent
menstruation (amenorrhea). Blood tests often reveal hormonal imbalance.
In
many women who have the disorder the ovaries are enlarged and feature numerous
small cysts along the outer edge of each ovary
A Mysterious Syndrome
Doctors don’t fully understand the exact
cause of polycystic ovary syndrome, but some of the following factors likely
play a role:
It’s believed that the majority of women
who have PCOS are compromised by a hormonal imbalance known as insulin
resistance. That means the body resists the workings of the hormone insulin,
whose job it is to get sugar channeled from the bloodstream to all of the
tissues and organs, where it’s needed for energy. To overcome the resistance,
more insulin is secreted, and many of the symptoms of PCOS are thought to be
the result of excess levels of this hormone. For instance, according to
Stanford University insulin expert Gerald Reaven, MD, too much insulin causes
the ovaries to manufacture abnormally high levels of the male hormone
testosterone, which in turn contributes to irregular menstruation. The high
testosterone levels are also to blame for the ovarian cysts (that can interfere
with fertility, excess facial hair, acne, and male-pattern hair thinning seen
in some women with PCOS, as well as the tendency for these women to store
excess body fat in their abdomens, like men. Research shows that excess
abdominal fat only further aggravates insulin resistance and thereby worsens
the symptoms of PCOS.
Low-grade inflammation. Your body’s white blood cells produce substances to fight infection
in a response called inflammation. Eating certain foods can trigger an inflammatory
response in some predisposed people. When this happens, white blood cells
produce substances that can lead to insulin resistance and cholesterol
accumulation in blood vessels (atherosclerosis). Atherosclerosis causes
cardiovascular disease. Research has shown that women with PCOS have low-grade
inflammation.
Heredity. If
your mother or sister has PCOS, you might have a greater chance of having it,
too. Researchers also are looking into the possibility that mutated genes are
linked to PCOS.
Abnormal fetal development. Some research shows that excessive exposure to male hormones
(androgens) in fetal life may permanently prevent normal genes from working the
way they’re supposed to – a process known as gene expression. This may promote
a male pattern of abdominal fat distribution, which increases the risk of
insulin resistance and low-grade inflammation. Researchers continue to
investigate to what extent these factors might contribute to PCOS.