You are 11 Weeks and 3 Days 200 days to go…
Does your face resemble the pimply complexion of your teenage years? Don’t worry, it’s those hormones again and it will pass.
Your baby today
As the baby floats in the amniotic fluid, her limbs are now more
fully developed, allowing her to make many movements. The lips and
fingers—which are now completely separated—stimulate sensory feelings.

Your skin is likely to change during pregnancy.
Some women find that they develop pimples or acne, due to the high
levels of progesterone. Conversely, you may get dry skin, also due to
pregnancy hormones. The dryness may become worse over your abdomen as
your belly grows and the skin is stretched.
Freckles and moles may get darker. You may also notice tiny red lines on your chest or legs: these are called spider nevi and are due to the increased blood supply to the skin which makes the vessels dilate and become more visible.
Other women find that
the high levels of estrogen mean that their skin is in a better
condition than before they were pregnant. The “glow” of pregnancy is due
to the increased blood supply that occurs in pregnancy, which gives you
a rosy healthy looking complexion.
Your skin may become dry and flaky, on your face, as well as elsewhere on your body. Using a good moisturizer should help.

… Doctor
| Q: |
Since going to the scan my partner is very overprotective. Is this normal?
|
| A: |
Your partner is now realizing his responsibilities and
affection for the baby, and is showing these feelings by taking care of
you. If you’re finding that his pampering of you is a little too much,
you might want to discuss other ways he can feel involved in the
pregnancy and prepare for the baby. Try to embrace his involvement and
enthusiasm—it’s a great way for you to strengthen your relationship and
prepare for parenthood together.
|
Telling your employer
As soon as your
employer knows you’re pregnant, you should be protected by the Pregnancy
Discrimination Act, which says that pregnant employees must be treated
the same as other employees with disabilities or limitations. Most
parents-to-be wait until 12 weeks when the risk of miscarriage is lower.
Some wait longer.
Each company has its own policy
on maternity leave. Some offer paid or unpaid leave for a set period.
Others let employees use sick leave or vacation days. Meet with a human
resources representative to learn your options.
You can discuss
when your maternity leave will start. If your baby is born early or
your maternity leave starts earlier than planned due to illness, the
arrangements can be altered at short notice.
Your employer
should respect your right to confidentiality. If you want the news of
your pregnancy to remain under wraps until a certain date, make this
known.
You are 11 Weeks and 4 Days 199 days to go…
At around 12 weeks, the doctor might be able to hear your baby’s heartbeat with a handheld monitor.
Your baby today
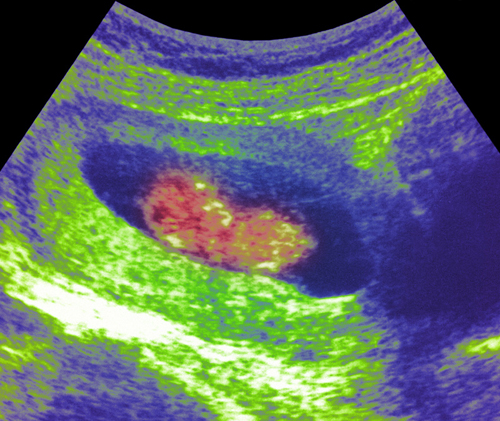
The fetus can be seen inside the uterus on this color ultrasound
scan. At this stage of development, the fetus measures approximately
2.4 in (6 cm) crown to rump and weighs around 0.3 oz (10 g).
At this stage your baby’s heart beats
at approximately 140 beats per minute, so at least twice as fast as
your own. The heart and its internal electrical conducting system are
structurally complete but its external nerve supply is still quite
immature. The nerves to the heart influence its rhythm, gradually
slowing the rate as the pregnancy advances.
The heart is tiny and
to maintain an adequate output the heart is unable to increase the
amount of blood it pumps with each beat (as we can), but instead
increases the number of times it beats each minute.
The abdominal cavity is
large enough to hold the intestines. Whereas before they were bulging
outside of your baby’s body, they now fit into her abdominal cavity.
Having started to rotate while outside the body, the bowel completes its
final rotation in the abdominal cavity. Once inside, the bowel position
remains fixed, and its diameter increases as the loops of bowel become
hollow.
Smoking: the facts
If you’ve only cut down, rather than quitting, read on.
Many smokers inhale more deeply when smoking less and their intake of
damaging toxins increases. Here’s how smoking affects your baby:
The carbon monoxide, nicotine, and other substances that you inhale pass from your lungs, into your blood-stream, and cross the placenta.
Nicotine makes your baby’s heart beat faster as she struggles for oxygen, which can affect her growth rate.
Smoking increases the risk
of miscarriage, premature birth, and low birth weight, and exposure to
tobacco chemicals makes your baby more likely to suffer from conditions
such as asthma and chest infections after the birth, which may be bad
enough to warrant a hospital stay.
There is also a higher risk of crib death if you or your partner smokes. Your partner should stop too.
If you live with a smoker,
you will be inhaling thousands of toxic carcinogenic chemicals that are
released into the air around you from the burning end of the cigarette
and the exhaled smoke.
Several studies have confirmed that passive smoking can damage the baby’s health and increase the risk of miscarriage and premature birth.
… Twins
Feeding two?
If you’re carrying twins,
you’re likely to have put on some weight by now, perhaps around 11 lb
(5 kg). Early weight gain is usually a good thing, especially in your
case, since this is a vital time for the formation and development for
your babies organs. As a rough guide, a good recommended weight gain is:
For twins, total weight gain of 35–45 lb (16–20 kg), preferably 24 lb (11 kg) by week 24, then a gradual increase until the birth.
For triplets, a total weight gain of 50–60 lb (23–27 kg), preferably 35 lb (16 kg) by week 24, then a gradual increase until the birth.
For quads, total weight gain of 65–80 lb (31–36 kg), ideally 50 pounds of it by week 24.

Screening Tests
Optional routine
screening tests in the first trimester assess the risk of your baby
having a chromosomal disorder such as Down syndrome.
What is screened for
In addition to Down
syndrome, screening tests also assess the risk of another chromosomal
abnormality called trisomy 18. Babies with this condition have more
severe mental and physical abnormalities than babies with Down syndrome
and seldom survive beyond a year. The condition is rare, with each year
around 1 in 6000 babies born with trisomy 18, compared to 1 in 800
babies born with Down. Screening can also detect neural tube defects
like spina bifida and anencephaly, which occur in about 1 in 1000
pregnancies.
The “combined” test
The recommended screening
test, and the one most commonly offered, for Down is the “nuchal
translucency screening,” performed between 11 and 14 weeks. This test
has a high accuracy rate and the results are produced quickly.
The test uses a
combination of a maternal blood test and an ultrasound of your baby. The
ultrasound measures the thickness of the skin at the back of your
baby’s neck, called the nuchal fold (see Nuchal translucency screening).
The blood test looks at the levels of two chemicals: pregnancy
associated plasma protein A (PAPP-A) and one of the pregnancy hormones,
human chorionic gonadotrophin (hCG). The results of the blood test is
combined with your age, and the measurement of the nuchal fold. A
mathematical formula is then used to calculate your baby’s risk of Down
syndrome.
If you have your blood
test before your ultrasound, you will usually receive your results
immediately following your ultrasound. If you have your blood drawn at
the time of the ultrasound you will receive your results a few days
later. Your risk based on the combined test may be higher than your risk
based on your age alone, lower, or stay the same.
The integrated test
This test is done in two
stages using results from a range of screening tests done in the first
and second trimesters. Your age will also be taken into account when
calculating your risk. In the first trimester, a blood test at 12 weeks
measures the PAPP-A and hCG. You will also have a nuchal translucency
screening. At between 15 and 22 weeks, another blood test measures the
levels of hCG, AFP, inhibin A, and estriol. The integrated test is the
most sensitive screening test, but it has the disadvantage that the
results are not available until later in pregnancy. It is not available
everywhere.
Triple and quadruple tests
These screening tests are
done in the second trimester, usually between 15 and 20 weeks
gestation, and assess your baby’s risk of Down syndrome from blood tests
alone. The triple test measures levels of the hormones hCG, AFP and
estriol. The quadruple test measures levels of inhibin-A in addition to
these three hormones. If your doctor or hospital doesn’t offer a nuchal
translucency screening, then a triple or quadruple test will be offered
instead.
A positive screen
It’s important to
remember that a positive result does not mean your baby has Down
syndrome. For example, if you have a 1 in 100 risk of Down syndrome,
your test will be positive. However, the chance that your baby has Down
syndrome is low since your baby will be normal 99 times out of 100.
Talking to your doctor or a genetic counselor can help you understand
your actual risk and decide if you want to have a diagnostic test such
as amniocentesis
for a definite result. Since diagnostic tests carry a risk of
miscarriage, you need to weigh the risks before deciding to go ahead.
Some research
suggests that women are more likely to enjoy their pregnancy and birth
and come to terms with the diagnosis if they know in advance that their
baby has Down syndrome. So don’t assume therefore that you should only
have a diagnostic test to decide whether or not to continue your
pregnancy.
If you have a positive
screening test for another more severe chromosomal disorder, such as
trisomy 18, your doctor will talk to you about the outlook for babies
with these conditions—the majority of whom die early in life, sometimes
within the first week—to help you decide what to do. In some cases these
disorders are associated with abnormalities detected during the dating scan,
and the presence of these abnormalities combined with a positive test
may confirm the diagnosis. Nevertheless, many women opt to have a
diagnostic test before deciding whether or not to terminate their
pregnancy.
Further screening
Another option
is to have a specialized ultrasound scan to look for Down syndrome
markers between 17 and 22 weeks. If the ultrasound doesn’t show any
signs of Down syndrome, the risk of your baby being affected is reduced.
However, a second trimester ultrasound is not such an accurate test for
Down syndrome as other screening tests and so you should only consider
this path if you are strongly against having a diagnostic test such as
amniocentesis and feel that you don’t need a definite diagnosis.
Understanding tests
Accuracy of screening tests
As more screening tests have become available,
the detection rate for Down syndrome, which used to be assessed on
maternal age alone, has significantly increased. The aim of screening
tests is to provide a high detection rate for Down syndrome and a low
“false positive” rate. A false positive means the screening test
indicated a high risk of Down syndrome, but subsequent diagnostic tests
gave the all clear, which means the mother would exposed to unnecessary
testing.
Table
| Tests | Timing (weeks) | Detection rate | False positive rate |
|---|
| Combined test | 11–14 | 85% | 5% |
| Integrated test | 11–13/15–22 | 85% | 1% |
| Quadruple test | 15–22 | 76% | 5% |
| Triple test | 15–20 | 69% | 5% |
Nuchal translucency screening
An ultrasound scan, known as the nuchal translucency screening, is done between 11 and 14 weeks
of pregnancy and is used to help assess your baby’s risk of Down
syndrome. During this test, the sonographer measures the depth of fluid
under the skin at the back of the baby’s neck, known as the nuchal fold.
If this measurement is high, it indicates that excess fluid is present,
which means that the baby has a higher risk of Down syndrome. The
measurement is then combined with the results of blood tests and the
average risk based on your age to give your baby’s individual risk for
Down syndrome. If your risk is higher than 1 in 250, you will be
counseled and offered a diagnostic test, such as amniocentesis or
chorionic villus sampling, to give a definitive result .
The small depth of fluid seen in the neck’s nuchal fold in this scan means that the fetus has a low risk of developing Down syndrome.

The thicker nuchal fold seen here indicates an increased risk of Down syndrome in this fetus and a diagnostic test will be recommended.

Should I have a diagnostic test?
Deciding on whether or not to go ahead with genetic or diagnostic testing is a personal choice. Factors that may affect your decision–making process include:
Your anxiety level without knowing for sure, and how this will affect your enjoyment of pregnancy.
Your fears about pregnancy loss.
What you would do if you found out your baby had Down syndrome or another condition such as Trisomy 18.