9. You Should Also Know
Weight Gain during Pregnancy
The amount of weight women gain during
pregnancy varies greatly. It may range from weight loss to a total gain
of 50 pounds or more, so it’s difficult to set one figure as an “ideal”
weight gain during pregnancy. But experts agree—gain the recommended
weight during pregnancy to have a healthier pregnancy.
How much weight you gain is influenced by your prepregnancy weight. Experts agree that what you weigh before pregnancy is the best indicator of how much weight you should gain during pregnancy. In addition, if you’re shorter than 5'2" tall, try to gain at the lower end of your weight range.
Statistics show nearly 45% of all pregnant
women gain more weight than they should. If you do, your risk of
problems goes up. You also put your baby at risk. And your child has a
much higher risk of being overweight by age 7.
Pregnancy Weight Gain
| Weight before Pregnancy |
Recommended Gain (pounds) |
| Underweight |
28 to 40 |
| Normal weight |
25 to 35 |
| Overweight |
15 to 25 |
| Obese |
11 to 20 |
| Morbidly obese |
Your healthcare provider will determine weight gain |
Another way to figure how much weight
you should gain during pregnancy is to look at your BMI (body mass
index). BMI guidelines for weight gain during pregnancy include the
following:
|
• BMI of less than 18.5—gain between 28 and 40 pounds |
|
• BMI of 18.5 to 25—gain between 25 and 35 pounds |
|
• BMI of 26 to 29—gain between 15 and 25 pounds |
|
• BMI of 30 or more—gain between 11 and 20 pounds |
|
• BMI of 40 and over—healthcare provider will determine weight gain |
Many experts call for a weightgain figure
of ⅔ of a pound (10 ounces) a week until 20 weeks, then 1 pound a week
from 20 to 40 weeks. Other researchers have set up weight-gain
guidelines for underweight, normal weight, overweight and obese women.
Nearly half of all
women who get pregnant have had a weight problem before pregnancy. You
shouldn’t diet while you’re pregnant, but that doesn’t mean you
shouldn’t watch what you eat. You should! Your baby will get proper
nutrition from the foods you eat.
Research shows if you dieted a lot before
pregnancy, you may gain more weight than recommended during pregnancy,
so pay strict attention to your eating plan. Choose foods for the
nutrition they provide for you and your growing baby. Watch your stress
levels, and try not to get too tired. If you’re stressed, fatigued or
anxious, you may eat more fats, sweets and junk-food snacks. This can
lead to an unhealthy amount of weight gain during pregnancy.
If you want to breastfeed, gaining more
weight than you should may contribute to breastfeeding problems. The
extra weight may also delay your milk from coming in.
If you have any
questions, discuss them with your healthcare provider. He or she can
advise you on how much weight you should gain during your pregnancy.
10. Ectopic (Tubal) Pregnancy
In a normal pregnancy, fertilization
occurs in the Fallopian tube and the fertilized egg travels through the
tube to the uterus. There it implants on the cavity wall.
An ectopic pregnancy occurs in the first 12 weeks of pregnancy when the egg implants outside
the uterine cavity, usually in the tube. Ninety-five percent of all
ectopic pregnancies occur in the Fallopian tube (hence the term tubal pregnancy).
We have seen the number of ectopic
pregnancies almost triple since 1985. Today about 7 in every 1000
pregnancies is ectopic. The reason for the increase? Researchers believe
STDs (sexually transmitted diseases) are the cause, especially
chlamydia and gonorrhea. If you have had an STD, tell your healthcare
provider at your first prenatal visit. And be sure to tell him or her if
you have had a previous ectopic pregnancy; there’s a 12% chance it will
happen again.
Chances of having an
ectopic pregnancy increase with damage to the Fallopian tubes from
pelvic inflammatory disease (PID), other infections, infertility,
endometriosis and tubal or abdominal surgery. Smoking, exposure to DES
(diethylstilbestrol) during your mother’s pregnancy and being older may
also increase your risk. Use of an IUD also increases the chance of
ectopic pregnancy.
Symptoms of ectopic pregnancy include:
• cramps or low-back pain
• tenderness in the lower abdomen
• bleeding or brown spotting
• shoulder pain
• weakness, dizziness or fainting caused by blood loss
• nausea
• low blood pressure
Diagnosing Ectopic Pregnancy. To test for ectopic pregnancy, human chorionic gonadotropin is measured. The test is called a quantitative HCG.
The level of HCG increases rapidly in a normal pregnancy and doubles in
value about every 2 days. If HCG levels do not increase as they should,
an ectopic pregnancy is suspected.
Ultrasound testing is helpful. An ectopic pregnancy may be visible in the tube. Blood may be seen in the abdomen.
We are better able to diagnose ectopic
pregnancy with laparoscopy. Tiny incisions are made in the area of the
bellybutton and in the lower-abdomen area. Healthcare providers look
inside the abdomen at the pelvic organs with a small instrument called a
laparoscope. They can see an ectopic pregnancy if one is present.
It’s best to diagnose a tubal pregnancy
before it ruptures and damages the tube. This could make it necessary to
remove the entire tube. Early diagnosis also tries to avoid the risk of
internal bleeding from a ruptured tube.
Dad Tip
You may be a happier camper if you help
out around the house more during your partner’s pregnancy. It can make
your life and hers easier if you pitch in to do some of the shopping and
household chores. Making your home safe for her also makes it safe for
your baby.
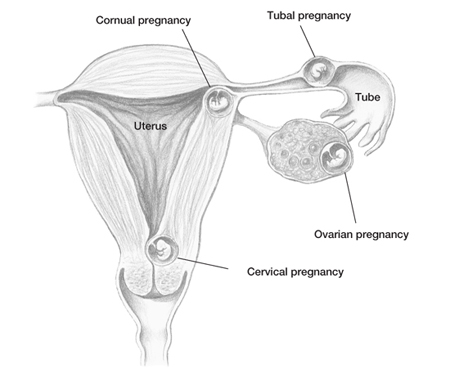
Possible locations of an ectopic pregnancy.
Most ectopic
pregnancies are detected around 6 to 8 weeks of pregnancy. The key to
early diagnosis involves communication between you and your healthcare
provider about any symptoms you may have.
Treatment for Ectopic Pregnancy.
The goal is to remove the pregnancy while maintaining fertility.
Surgery requires general anesthesia, laparoscopy or laparotomy (a larger
incision and no scope) and recovery from surgery. In many instances,
the Fallopian tube may need to be removed, which may affect future
fertility.
A nonsurgical
treatment involves the use of a cancer drug, methotrexate. It is given
by I.V. in the hospital or at an outpatient clinic. Methotrexate ends
the pregnancy. HCG levels should decrease after this treatment, and
symptoms should improve. If methotrexate is used to treat an ectopic
pregnancy, a couple should wait at least 3 months before trying to
conceive again.
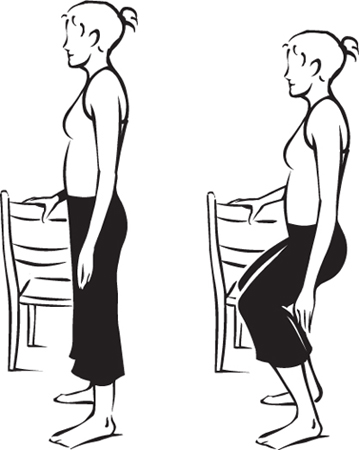
10. Exercise for Week 5
Lightly grasp the back of a chair or a
counter for balance. Stand with your feet shoulder-width apart. Keep
your body weight over your heels and your torso erect. Bend your knees,
and lower your torso in a squatting position. Don’t round your back.
Hold the squatting position for 5 seconds, then straighten to starting
position. Start with 5 repetitions and work up to 10. Strengthens hip, thigh and buttocks muscles.