Amniocentesis
Amniocentesis is a test done on fetal
cells and is often offered to women over 35 or women whose
screening-tests results are abnormal. Most women who have amniocentesis
are being screened for chromosomal defects, such as Down syndrome,
Turner’s syndrome or neural-tube defects (spina bifida). The test can
pick up some specific gene defects, including cystic fibrosis and
sickle-cell disease. Other problems the test can identify include:
•skeletal diseases, such as osteogenesis imperfecta
•fetal infections, such as herpes or rubella
•central-nervous-system disease, such as anencephaly
•blood diseases, such as erythroblastosis fetalis
•chemical problems or deficiencies, such as cystinuria or maple-syrup-urine disease
•fetal sex, if sex-specific problems, such as hemophilia or Duchenne muscular dystrophy, must be identified
Amniocentesis may be performed to
determine if the baby of an Rh-negative woman is having problems. It
may also be done to determine fetal lung maturity before delivery.
It may be a good idea to have
amniocentesis if your healthcare provider suggests it, even if you
would not end your pregnancy should results indicate a problem. If a
problem is detected, you and your family can prepare for it. You can
gather information about the problem so you and your family are
informed about what lies ahead.
Amniocentesis near the end of pregnancy can determine if a baby’s lungs are mature.
The test may also indicate the need for
additional tests to determine if the fetus might have other problems.
If any are found, steps can be taken to ensure the delivery goes
smoothly and any necessary procedures are done as soon after the birth
as possible.
Not every pregnant woman needs amniocentesis. It is often performed on women who fit any of the following criteria:
•they will deliver after their 35th birthday
•they have had a previous baby with a birth defect
•they have a family history of birth defects
•they have a birth defect themselves
•their partner has a birth defect
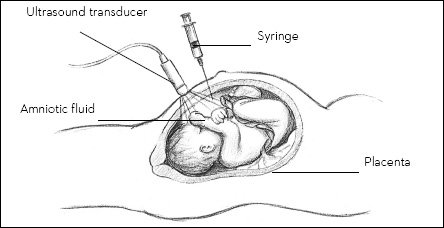
Ultrasound is used to locate a pocket of
fluid where the fetus and placenta are out of the way. Skin over the
mother’s abdomen is cleaned and numbed with a local anesthetic. A
needle is passed through the abdomen into the uterus, and fluid is
withdrawn with a syringe. About 1 ounce (30g) of amniotic fluid is
needed to perform the tests. The test can identify about 40 fetal
abnormalities.
Bleeding from the fetus to the mother can
occur during amniocentesis, which can be a problem because fetal and
maternal blood are separate and may be different types. This is a
particular risk to an Rh-negative mother carrying an Rh-positive baby
and may cause isoimmunization. An Rh-negative woman should receive
RhoGAM at the time of amniocentesis to prevent isoimmunization.
Amniocentesis in a Multiple Pregnancy
In a multiple pregnancy, genetic
testing can be a complicated procedure. For example, in most multiple
pregnancies, each baby lies in its own sac. Abdominal punctures are
required to withdraw fluid from each sac, which can increase the risk
of complications. In the case of one sac shared by the two babies, only
one puncture is necessary.
Over 95% of women who have amniocentesis learn their baby does not
have the disorder the test was done for. Fetal loss from amniocentesis
complications is estimated to be less than 3%. Discuss the risks with
your healthcare provider before the test. Only someone with experience,
such as a physician at a medical center, should perform the test.
A disadvantage of amniocentesis
is the time at which it is performed. Amniocentesis is usually
performed for prenatal evaluation at around 16 weeks of pregnancy,
making termination of a pregnancy (if that is what the woman chooses)
more difficult. Some healthcare providers perform the test at around 11
or 12 weeks. However, not everyone agrees this early use is beneficial.