1. How Big Is Your Baby?
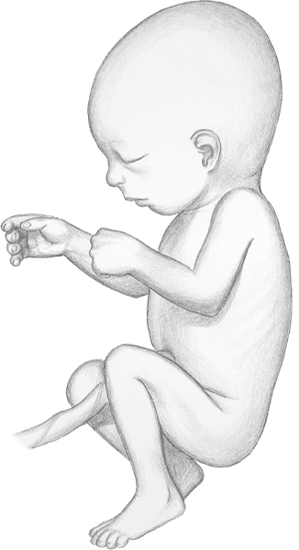
By this week, baby weighs almost
1 pound (455g)! Its crown-to-rump length is 8 inches (20cm). Your baby
is about the size of a small doll.
2. How Big Are You?
Your uterus extends about 1½ inches
(3.75cm) above your bellybutton or about 9¼ inches (23cm) from the
pubic symphysis. Your total weight gain should be between 12 and 15
pounds (5.5 and 6.8kg).
3. How Your Baby Is Growing and Developing
Baby’s body is getting plumper but skin is still wrinkled.
Lanugo hair on the body occasionally turns darker at this time. The
baby’s face and body begin to assume more of the appearance of an
infant at birth.
Your baby’s pancreas is important in
insulin production. Insulin is necessary for the body to break down and
to use sugar. When the fetus is exposed to high blood-sugar levels from
the mother-to-be, its pancreas responds by increasing the blood-insulin
level. Insulin has been identified in a fetal pancreas as early as 9
weeks of pregnancy and in fetal blood as early as 12 weeks.
Blood-insulin levels are generally high
in babies born to diabetic mothers. This is one reason your healthcare
provider may monitor you for development of gestational diabetes.
Twin-to-Twin Transfusion Syndrome (TTTS)
Twin-to-twin transfusion syndrome (TTTS) occurs only in identical twins who share the same placenta. The syndrome is also called chronic intertwin transfusion syndrome. The condition can range from mild to severe and can occur at any point during pregnancy, even at birth.
Dad Tip
Are you also having pregnancy symptoms?
Studies show as many as 50% of all fathers-to-be experience physical
symptoms of pregnancy when their partner is pregnant. Couvade,
a French term meaning “to hatch,” is used to describe the condition in
a man. Symptoms for an expectant father may include nausea, weight gain
and cravings for certain foods.
TTTS cannot be prevented; it’s not a
genetic disorder nor a hereditary condition. We believe it occurs in 5
to 10% of all identical-twin pregnancies. TTTS occurs when twins share
a placenta. These problems do not occur in twins who each have a
placenta.
In TTTS, twins also share some of the
same blood circulation. This allows the transfusion of blood from one
twin to the other. One twin becomes small and anemic. Its body responds
by partially shutting down blood supply to many of its organs,
especially the kidneys, which results in reduced urine output and a
small volume of amniotic fluid.
The other twin grows large, overloaded
with blood. It produces excessive amounts of urine so it is surrounded
by a large volume of amniotic fluid. Because the recipient twin has
more blood, it urinates more and has more amniotic fluid. Its blood
becomes thick and difficult to pump through its body; this can result
in heart failure.
The twins are often very different in
size. There can also be a large difference in their weights. TTTS is a
progressive disorder, so early treatment may prevent complications.
Symptoms of TTTS.
There are symptoms of the syndrome your health care provider looks for.
If your abdomen enlarges quite rapidly over a 2- to 3-week period, it
may be caused by the buildup of amniotic fluid in the recipient twin.
The result can be premature labor and/or premature rupture of
membranes. If one twin is small for its gestational age or one is big
for its gestational age, it may indicate TTTS. In addition, your
healthcare provider may suspect TTTS if any of the following is seen
during an ultrasound:
By the 23rd week of pregnancy
(fetal age—21 weeks), your baby’s eyelids
and eyebrows are well developed.
• large difference in the size of fetuses of the same gender
• difference in size between the two amniotic sacs
• difference in size of the umbilical cords
• one placenta
• evidence of fluid buildup in the skin of either fetus
• indications of congestive heart failure in the recipient twin
An additional problem may develop in
either twin. With this condition, fluid accumulates in some part of the
fetus, such as in the scalp, abdomen, lungs or heart.
Diagnosing and Treating TTTS. Report any of the following to your healthcare provider, especially if you know you’re expecting twins:
• rapid growth of your uterus
• abdominal pain, tightness or contractions
• sudden increase in body weight
• swelling in the hands and legs in early pregnancy
The syndrome may also be detected with
ultrasound examination of the uterus. It’s important to find out
whether twins share the same placenta, preferably in the first
trimester because in the second trimester it can be harder to learn
whether they share one placenta.
If the syndrome is mild or undetected on
ultrasound, the appearance of the twins at birth may identify it. A
complete blood cell count done after birth will show anemia in one twin
and excess red blood cells in the other.
If diagnosed, the Twin to Twin
Transfusion Syndrome Foundation recommends weekly ultrasounds after 16
weeks till the end of the pregnancy to monitor TTTS. They recommend
this be done even if the warning signs of TTTS have decreased.
The most common treatment for TTTS is
amnioreduction, in which large volumes of amniotic fluid are drained
from the sac of the larger twin. A needle is placed through the
mother’s abdomen, and fluid is drained. The procedure is repeated, if
necessary.
In another
procedure, a hole punched between the two amniotic sacs can help
equalize the fluid between the sacs. However, neither of these
procedures stops the twin-to-twin transfusion.
Some cases of TTTS do not respond to
amnioreduction. A small-scope laser procedure may be done to seal off
some or all of the blood vessels the twins share. Usually only one
procedure is necessary during the pregnancy. Survival rates are also
about 60% with this procedure. This treatment is most successful if
done before 26 weeks of pregnancy.
With the laser treatment, a detailed
ultrasound exam is done first to help locate the abnormal connection.
Then a thin fiber-optic scope is placed through the mother’s abdomen,
through the wall of the uterus and into the amniotic cavity of the
larger twin. By looking directly at the placenta, blood connections can
be found and sealed by directing a laser beam at them. This separates
the circulation of the fetuses and ends twin-to-twin transfusion.
However, this requires doing the procedure while the babies are still
in the womb and may cause serious complications.
The most conservative treatment is to
watch and to wait. The pregnancy is followed closely with frequent
ultrasound examinations, with the choice of delivering the twins by
Cesarean delivery if medically necessary.
Newborns with twin-to-twin transfusion
syndrome may be critically ill at birth and require treatment in a
neonatal intensive care unit. The smaller twin is treated for anemia,
and the larger twin is treated for excess red blood cells and jaundice.