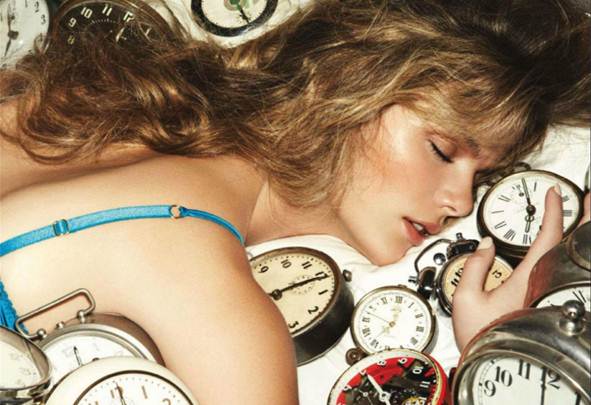
Ten million sleeping-pill prescriptions are
written in the UK every year.
On the second shelf of my bathroom cabinet,
behind a jar of hair mask, lies a small plastic box containing one Xanax and 12
zopiclone bought in a chemist in Egypt. They’re the final remnants of my
ten-year addiction to sleeping pills that almost led to a trip to A&E.
Despite begging several GPs for help over the years, I’ve been repeatedly let
down by our healthcare system, making me feel my crippling dependency looked
like attention-seeking. I’m finally on the (slow) road to recovery, thanks to a
bout of news stories earlier this year highlighting the dangers of sleeping
pills that jolted me into kicking my habit for good.
I’m
addicted to sleeping pills
One morning in February, after another
sleepless night, I switched on my computer to find the news dominated by
headlines linking hypnotics (ie sleep-including drugs) to cancer, declaring
they could be more harmful than cigarettes. I felt sick reading that a new
study, led by long-time critic of sleeping pills Dr Daniel Kripke, found even
occasional sleeping pill-user were over four times more likely to die earlier
than non-users. It was exactly what I need to drastically change my lifestyle.
From the age of 12, I can remember entirely
sleepless nights. My grandmother had been a terrible insomniac and it was
always assumed I’d inherited it from her. In my twenties, I read all the
advice: I followed rigid regimes, eating and exercising at the correct times,
completely cutting out caffeine and alcohol, and trying an array of herbal
remedies, topical creams, over-the-counter sleeping remedies – even CDs of
dolphin sounds. Nothing worked. Days, even weeks, would pass with my getting
just an hour’s sleep each night. Other times, I hadn’t slept at all when my
morning alarm shrieked to life.

About
nine years ago, I had three particularly unbearable nights, prompting me to
visit my GP for the first time
Too tired to make it into work, I began
regularly calling in sick, making up wild excuses – everything from household
emergencies to migraines, even tropical illnesses – researching symptoms on the
internet to make them seem plausible.
About nine years ago, I had three
particularly unbearable nights, prompting me to visit my GP for the first time.
He prescribed the sedative diazepam (another name for Valium) to help induce
sleep and effectively knock me out. It did. I took one tablet every day for two
weeks and it was like being a new person; this is what it felt like to sleep. I
was wide awake and alerts during the day and no longer needed layers of
concealer to cover the bags under my eyes. I was convinced these pills were the
solution to my long struggle with sleep. When they ran out, I went back for
more. He warned they could become addictive and was reluctant to give me a
longer prescription, so I started seeing different GPs in my surgery, asking
for extra pills.
None of my doctors seemed to understand the
devastating effect insomnia had on my life. Every request for a referral to a
sleep specialist was rebuffed. I was told that sleep clinics were only for
patients with ‘serious’ problems, such as sleep apnoea, a condition that causes
people to stop breathing during sleep.
The notion that insomniacs don’t ‘try’ to
sleep is all too familiar. It’s hard to comprehend the frustration and fear I
feel lying awake until dawn, night after night, ‘trying’ to no avail. Sometimes
I’d get so frustrated I’d burst into angry, hot tears and wake my husband,
David, up for support.

None
of my doctors seemed to understand the devastating effect insomnia had on my
life
The problem is not necessarily stress
related, but simply comes out of nowhere. I’ll sleep well for weeks, then
suddenly a period of insomnia will hit me. One sleepless night is invariably
followed by another, as the anxiety about being some mentally tired and so
physically drained the following day keeps me awake.
Though doctors were sympathetic, it became
harder to get prescriptions. On holiday in India, I discovered you could buy
sleeping pills over the counter. I had to see a pharmacist for a cold, and he
offered me a decongestant and diazepam. I scoured several chemists near my hotel
and flew home with enough to last me a year. I didn’t take them every day, but
just knowing I had them made me less anxious about sleeping. I soon discovered
that conversations about where to stock up on the best sleeping drugs are
commonplace in airport lounges. I even started believing that taking them was
completely normal.
In 2008, my stash eventually ran out. My
new GP refused to prescribe my usual 28-pack of temazepam (similar to diazepam
but the effects wear off more quickly), giving me just seven, making it clear
he wouldn’t be prescribing any more and accusing me of wanting them to commit
suicide. His advice? “Try harder.”
Too scared to go back and ask for more, I
hit a new low. I had an early start at a new job and needed a good night’s
sleep, so I raided the medicine cabinet, taking everything labeled ‘may cause
drowsiness’ – including a prescription that my husband had been given for a
back injury.

The
following morning, I passed out on the train during my commute to work. One
minute I was standing up, the next I’d collapsed on top of a total stranger.
The following morning, I passed out on the
train during my commute to work. One minute I was standing up, the next I’d
collapsed on top of a total stranger. It was mortifying. David called the doctor’s
surgery who said I’d been extremely lucky that the cocktail of drugs I had
taken weren’t from the same family, otherwise I would have been in A&E
having my stomach pumped.