Monitoring During Labor
Throughout labor,
your baby’s heartbeat and your contractions will be monitored to make
sure that your labor is progressing as it should be and that the
well-being of you and your baby is not threatened.
Your baby’s heart rate is
an indication of how well your baby is dealing with labor and it is
monitored at regular intervals, called intermittent monitoring. If a
problem is found or you have a high-risk pregnancy, then you may be
advised to have fetal electronic monitoring, in which your baby’s heart
rate and your contractions are monitored continuously by a electronic
fetal heart monitor . All the information about your labor is recorded on a chart, called a labor graph.
A handheld device can monitor your baby’s heartbeat at intervals, leaving you free to move around during labor.

Intermittent monitoring
This is done using a
handheld battery-operated device known as a Doppler sonicaid, which is
held against your abdomen to listen to your baby’s heartbeat. When you
are pushing in the second stage of labor, the fetal heart needs to be
monitored more frequently.
Electronic fetal monitoring
In this type of fetal
monitoring, two devices monitor your baby’s heart rate and the strength
and frequency of your contractions. Your baby’s heart rate is monitored
with a circular ultrasound-like device. If you want, you can hear the
heartbeat, or ask that the volume be turned down if this is distracting.
Your contractions are monitored with a small plastic circular device.
One or two elastic belts are placed around your abdomen to secure the
monitors. You should be able to stand, sit, or squat with the monitors
in place, and some hospitals have monitors that allow you to walk around
and be monitored by radio signal.
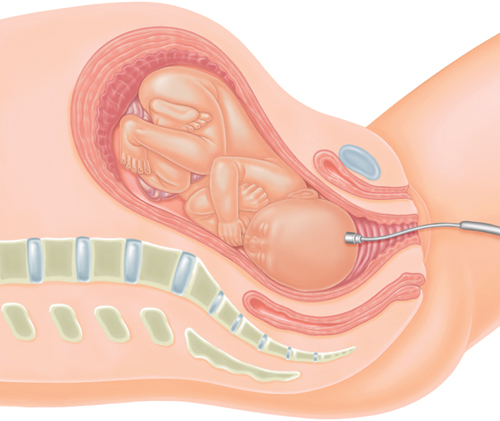
Internal monitoring
If your baby’s heart-rate
reading indicates the baby is distressed or the signal from an
electronic monitor is poor, the doctor may suggest internal fetal
monitoring. In this technique, a small electrode is attached to the
baby’s scalp and detects the electrical impulses of his heart. A wire
from the electrode comes out via the cervix and attaches to the EFM
machine (see External fetal monitoring). You still wear a strap around your abdomen, which holds the device for detecting the rate and strength of your contractions.
The electrode is
placed during a vaginal examination and is no more uncomfortable than
this. Placing a scalp electrode may be mildly uncomfortable for your
baby and there is a small risk that your baby could get a scalp
infection, which can be treated with antibiotics. Even though these
risks are small, a scalp electrode should not be placed routinely. Your
doctor should discuss how it works before it is placed, and you should
understand why it’s being done. Electrodes should also be avoided if you
have a viral disease that can be transmitted to your baby during labor,
such as hepatitis B or C, or HIV. Once a scalp electrode has been
placed, you can’t move far from the monitor, although you may be able to
change position.
If a EFM reading from
the scalp electrode indicates that your baby is distressed, a blood
sample may be taken from the scalp to check acidity levels. If these are
high, a cesarean or assisted delivery may be suggested.
Labor graphs
A labor graph is a large
chart that contains several graphs which provide information on your
labor, allowing the doctor to monitor the progress of your labor. One of
the most useful tools in this chart is a graph showing your labor
curve. This plots cervical change and the position of your baby’s head
in relation to your pelvis over time. The graph enables the doctor to
establish when your labor became active. Also recorded with your baby’s
heart-rate monitoring are your blood pressure, pulse, temperature, and
the rate of your contractions, as well as your pain levels.
How monitoring is done
External fetal monitoring
The baby’s heartbeat and the strength and frequency of your contractions
are measured by devices strapped to your abdomen with wires that
connect to a machine that produces a printout of the readings and an
ongoing digital log on the computer.
Your baby’s heartbeat
is recorded against a baseline measurement of 120 beats per minute. The
heart rate rises and falls naturally with contractions; unusual
variations can indicate fetal distress.
A separate reading
records the strength and duration of each contraction. This can detect
weakening contractions and can be useful with an epidural when you’re
unable to feel contractions.
Continuous monitoring of your baby’s heart rate and your contractions is done by means of monitors strapped to your abdomen.

Internal monitoring
Scalp electrode
If there are concerns
about the baby’s heartbeat, a small electrode attached to the scalp can
give a more precise reading than external electronic fetal monitoring
The electrode is passed through the cervix and attached to the head.
Should you have electronic fetal monitoring?
Although monitoring during labor is an important part of the care of you and your baby,
there is some debate as to the benefits of continuous monitoring and
some believe there may be associated maternal risks. As a result, most
hospitals suggest intermittent fetal monitoring. Although you can refuse
monitoring entirely, the staff may be unhappy about this and ask you to
sign a form or statement releasing them from liability if anything goes
wrong during the labor and birth.
Risks
Studies suggest that
women who are monitored continuously are more likely to have a cesarean
section or an assisted delivery with forceps or vacuum .
This is because your doctor may see changes in the fetal heart rate
that concern her. Some changes, such as a faster heart rate (more than
160 beats a minute), known as tachycardia, or decreases in the heart
rate that occur after your contractions, can be caused by decreased
oxygen to your baby. If your doctor sees these changes, she may be
unable to determine if they were caused by low oxygen or if your baby is
actually fine.
If it’s thought that your
baby may be at risk, an emergency cesarean section may be recommended.
If there are fetal heart rate changes while you are pushing, a forceps
or vacuum delivery may be offered.
Benefits
The
benefits of continuous electronic fetal monitoring are not entirely
clear. You are able to hear your baby’s heartbeat and some women may
find this comforting. Also, experts agree that continuous monitoring
reduces the chance that your baby will have a seizure after the birth, a
symptom of brain injury from low oxygen. Seizures are rare, occurring
in around 2.5 per 1000 births with monitoring and 5 per 1000 births
without monitoring. It is harder to prove that electronic fetal
monitoring can prevent rarer complications such as cerebral palsy or
fetal death.