When it comes to osteoporosis it’s never too
early to start protecting yourself. A few simple lifestyle changes are all it
takes
You trip, put out a hand to save yourself
and, without warning, you end up in plaster with a broken bone. It could happen
bone. It could happen to any of us. It’s painful, inconvenient and a very real
risk for the one in every two women over 50 who breaks a bone after a trivial
fall because of osteoporosis. “Healthy bones should be able to withstand a fall
from standing height,” says the National Osteoporosis Society (NOS). But from
our 30s onwards, being aware and making some simple lifestyle changes can help
us ensure that a break means a holiday and not a hospital stay.

Careful!
You can guard against unlucky breaks
1. Sleep soundly… but skip the lie-in
Keep your back in alignment by sleeping on
your side, or on your back with a pillow under your knees. Then set the alarm.
One study of 19,000 people found that those who slept for more than eight hours
a night were at higher risk of osteoporosis.

Sleep
soundly… but skip the lie-in
2. Eat greens – and not just spinach
Not all greens are equal. Watercress and
spinach contain oxalic acid, which blocks the update of calcium by the bones.
“Try kale, spring greens, and broccoli, which don’t have that effect,” explains
Sarah Leyland of the NOS.

Eat
greens – and not just spinach
3. Think slim, not skinny
A BMI of less than 19 is a risk factor for
osteoporosis: find yours with the BMI calculator on the NHS website (nhs.uk).
4. Ask about your mum’s health (and don’t forget your dad’s)
You may not realize it, but 80% of bone
health is inherited – so your mum’s broken hip could affect your health. But
having a father who fractures a bone, as one in five older men do, also
increases your risk.
5. Resist bone loss with the right workout
Weight training and Pilates with bands are
both types of resistance exercise, which tones muscles, strengthens bones and,
as a bonus, sees off batwings, too. If you’re fit and active, try for three
sessions a week, leaving a rest day in between to let your body recover. Can’t
stand the gym? Use your own body weight – press-ups can improve bone density in
the forearm, says the NOS. (If the mere thought makes you groan, start by doing
them against a wall.)
6. Skip the sunscreen – but just for 10 minutes
Sunshine provides 90% of the vitamin D our
bones need, so take advantage of it when it does appear. Aim for two 10-minute
sun breaks a day between May and September, without sunscreen, to allow skin to
soak up the sun and strengthen bones naturally.

A
little summer sun can give bones a boost
7. Dance, but don’t party
Dancing is a great way to protect your
bones, but avoid smoking and heavy drinking. Cigarettes and an alcohol intake
of more than two units a day both erode bone.
8. Keep a diary (But not like bridget jones)
Instead, track your periods, as it’s not
just fertility that’s affected if illness or weight loss interferes with
menstruation. Oestrogen produced during the cycle also protects our bones, so
any woman whose periods stop for six months or more should see her GP. If the
cause is premature menopause, HRT is usually prescribed until 52 – the average
age at which periods stop.
9. Worry less about weight and more about height
Osteoporosis is one condition where it’s
better to be heavier than lighter, says rheumatologist Professor David Reid of
the University of Aberdeen, because a few extra pounds may protect your bones.
In contrast, monitoring height is vital, as a subtle loss of inches is a sign
of compressed or fractured vertebrae in the spine. Check it every year after
your 50th birthday – losing more than 4cm (1½ inches) needs
attention.
10. Go for a
walk – and take the kids
Do their bones a favor and drag them away
from the iPad. Young girls, in particular, need plenty of exercise to build up
their ‘bone bank’ and prevent future problems. It’s especially important when
they start secondary school, because they create as much bone between the ages
of 11 and 13 as they will lose in the 30 years post-menopause.

Go
for a walk – and take the kids
11. Health
problems weaken bone, but so can the cure
Anyone with rheumatoid arthritis, type 1
diabetes, inflammatory bowel or coeliac disease, or an overactive thyroid
should be monitored for osteoporosis. And make sure you’re assessed if you’re
prescribed drugs for epilepsy or have taken steroids (prednisolone) for more
than three months.
12. Say no to
diet cola and yes to latte
Regular cola drinkers may be at greater
risk of bone loss, according to US research. But it’s the acidity-not the
caffeine- that’s to blame. Although high levels of coffee can lead to calcium
loss, it’s unlikely to harm bones unless you have more than five cups a day. To
be safe, drink it white. Just two tablespoons of milk per cup can help
neutralize the effect.
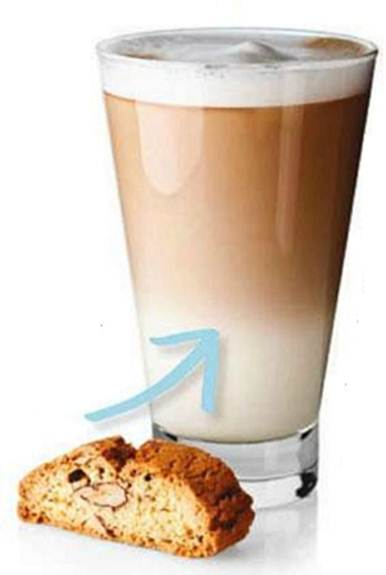
Say
no to diet cola and yes to latte
13. Be picky
with protein- unless it’s from plants
Most protein is acidic (but not in taste)
and leaches calcium from the bones- one reason why we’re advised to limit our
daily intake to 1.5g per kg of body weight (around 95g for a 10-stone woman).
The trouble is, we’re also supposed to eat 700g calcium a day and the best
sources are often high in protein. Try to balance animal protein. Try to
balance animal protein with alkaline foods such as protein – rich beans, fruit
and veg. But avoid calcium supplements unless you are medically advised to take
them.

Try
to balance animal protein. Try to balance animal protein with alkaline foods
such as protein – rich beans, fruit and veg.
14. Lean back,
not forward
If you’re at a high risk of osteoporosis,
swap sit- ups and toe touches for baby backbends. Too much forward movement can
put pressure on the spine, and if your back is fragile it could cause a
compression fracture. ‘Ask your instructor for alternatives, such as sit-ups
with a cradle,” says Sarah Leyland of the NOS, and take care when bending or
twisting during golf and tennis. Visit nos.org.uk to download its leaflet,
Exercise And Osteoporosis.
15. The pill
may help – but contraceptive jabs won’t
Taking the contraceptive pill can top up
the hormones needed to protect bones in women who have an early menopause. If
you simply want to prevent pregnancy, however, avoid injectable contraceptives,
which can make bones more fragile.
16. If you
break a bone, your GP should ask questions…
Funding is now available for GPs to assess
patients for bone strength following a fragility fracture, and NICE is
considering extending screening to all women over 65. But why wait? Work out
your risk for yourself using the Frax tool from The University of Sheffield
(visit shef.ac.uk/frax).