5. Changes in Your Skin
During pregnancy, many things can cause
changes in your skin, such as hormones and stretching skin. Below we
discuss some of the changes you may experience.
Skin-Color Changes.
Melanin cells in your skin produce pigment; hormones can cause your
body to produce more pigment. These may lead to a variety of skin-color
changes. Women of color may be at increased risk for changes in skin
color, which may leave the skin darker or lighter than it was before.
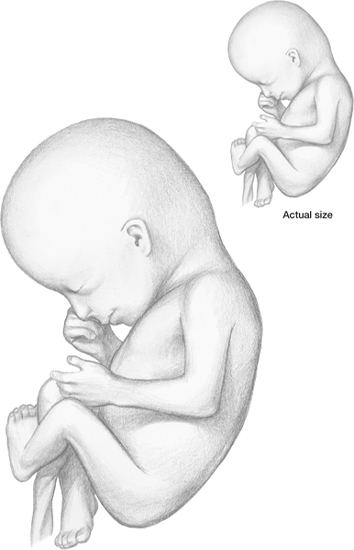
Your baby is growing rapidly. It has doubled
its length in the past 3 weeks.
Itchy Skin.
Pregnant women often have dry, itchy skin. Moisturizers can help, but
you can also help your skin by eating omega-3 fatty acids. They’re good
for you and baby. Olive oil, almonds and macadamia nuts contain omega-3
fatty acids, so eat these if you do not eat fish.
If you have sensitive skin and experience
itchy hives, try rubbing milk of magnesia on the affected area. Rubbing
it into the skin helps reduce itching.
Cholestasis of Pregnancy.
A sudden attack of itching on the palms and soles may indicate
cholestasis of pregnancy. Itching then spreads to the rest of the body.
Cholestasis of pregnancy, also called intrahepatic cholestasis of pregnancy (ICP) or prurigo gravidarum, is a condition in which a woman has severe itching all over the body, but there’s no rash.
The condition is rare. We see only about one case in 10,000 pregnancies in the United States.
Intense itching all over begins in the
third trimester. Usually it’s much worse at night. Other symptoms
include jaundice, light-colored stools and dark urine.
Treatment includes anti-itch creams and UVB light treatments. Symptoms generally disappear a few days after baby’s birth.
Chloasma. Occasionally irregular brown patches appear on the face and neck, called chloasma or mask of pregnancy.
These disappear or get lighter after delivery. Birth-control pills may
cause similar changes. Up to 70% of all pregnant women develop chloasma
after exposure to the sun. Women of Asian, Hispanic, North African,
Indian and Middle Eastern heritage are more prone to developing
chloasma.
The best way to prevent chloasma is to
stay out of the sun, especially during the hottest part of the day
(between 10am and 3pm). Wear sunscreen and protective clothing (hats,
long-sleeved shirts, long pants). Brown patches usually fade in the
months after delivery. If they don’t, ask your healthcare provider about
using Retin-A.
Plaques of Pregnancy (PUPP).
Some women have a severe, itchy rash of red bumps that begins on the
tummy and spreads to the lower body, then to the arms and legs. This is
called plaques of pregnancy, toxemic rash, polymorphic eruption of pregnancy or pruritic urticaria pappules (PUPP). With plaques of pregnancy, your healthcare provider may first rule out scabies.
PUPP is the most common skin problem
pregnant women experience; it’s more common in white women. It may be
caused by the skin stretching rapidly, which damages tissue, resulting
in bumps and inflammation.
This condition usually appears in first
pregnancies during the third trimester. It often affects women who gain a
lot of weight or those who are expecting multiples.
The good news is that PUPP won’t harm the
baby. The bad news is the itching can be so severe that relief may be
all you think about, especially at night, which may cause you to lose
sleep. PUPP usually resolves within a week of delivery and doesn’t
usually come back with future pregnancies.
Many treatments have been recommended for
relief, including Benadryl, powders, creams, calamine lotion, soaking in
cold tubs, oatmeal baths, witch hazel, going without clothes and
ultraviolet (UVB) therapy. If you can’t find relief, talk to your
healthcare provider. He or she may have some recommendations for home
remedies that have worked for other women. If all else fails, a
prescription for oral antihistamines, topical steroids or cortisone
cream may be needed.
Pemphigoid Gestationis (PG; Herpes Gestationis). Pemphigoid gestationis (PG)
usually begins with blisters around the bellybutton. It may occur in
the second or third trimester or immediately after birth. Despite its
name, PG has no relationship to the herpes simplex virus. The name came
about because the blisters appear similar to herpes infections. It
occurs in 1 in 50,000 pregnancies.
The problem begins with sudden onset of
intensely itchy blisters on the tummy in about 50% of cases. For the
other 50%, blisters can appear anywhere on the body. It often resolves
during the last part of pregnancy. It can flare up at delivery or immediately after baby’s birth, which happens more than 60% of the time.
The goal of treatment is to relieve
itching and to limit blister formation. Oatmeal baths, mild creams and
steroids are used. PG usually eases a few weeks after delivery and can
recur in your next pregnancies and with oral-contraceptive use. Infants
are not at risk.
Other Skin Changes. Vascular spiders (called telangiectasias or angiomas) are small red elevations on the skin, with branches extending outward. A similar condition is redness of the palms, called palmar erythema. Vascular spiders and palmar erythema often occur together. Symptoms are temporary and disappear shortly after delivery.
In many women, skin down the middle of the
abdomen becomes markedly darker or pigmented with a brown-black color.
It forms a vertical line called the linea nigra. It causes no problems and may be permanent.
Atopic eruption of pregnancy (AEP)
covers three different pregnancy skin conditions that cause
itching—eczema of pregnancy, prurigo of pregnancy and pruritic
folliculitis of pregnancy. If you experience eczema, you may need
prescription skin cream. Research has shown that Elidel and Protopic
may have a potential risk for causing cancer. Don’t use either to treat
diaper rash or any other type of rashes in baby.
Prurigo of pregnancy is a poorly
understood pregnancy skin condition. It may look like insect bites, and
it itches. Treatment includes anti-itch creams and steroid creams. The
condition usually resolves after delivery. There’s no risk to you or
baby.
Pruritic folliculitis of pregnancy
(PFP) occurs in the second and third trimesters. It usually appears as
an elevated, red area in hair follicles on the chest and back. Usually
some mild itching is involved; the problem resolves 2 to 3 weeks after
delivery.