1. How Big Is Your Baby?
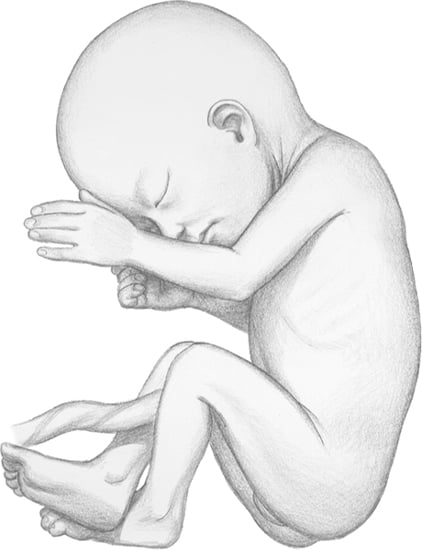
Your baby weighs about 12¼ ounces (350g). Crown-to-rump length at this time is about 7 ⅔ inches (19cm).
2. How Big Are You?
Your uterus is about ¾ inch
(2cm) above your bellybutton. Your growing tummy doesn’t get in your
way much; you may feel pretty good. You’re still able to bend over and
to sit comfortably. Walking shouldn’t be an effort. Morning sickness
has probably passed. It’s kind of fun being pregnant now!
3. How Your Baby Is Growing and Developing
Your baby’s organ systems are becoming
specialized for their particular functions. Consider the liver. The
function of the fetal liver is different from that of an adult.
Chemicals are made in an adult liver that are important in various body
functions. In the fetus, chemicals are present but in lower amounts.
An important function of the liver is
managing bilirubin, which is produced by the breakdown of blood cells.
The life span of a fetal red blood cell is shorter than that of an adult. Because of this, a baby makes more bilirubin than an adult does.
The fetal liver has a limited capacity to
change bilirubin and remove it from baby’s bloodstream. Bilirubin
passes from fetal blood through the placenta to your blood. Your liver
helps get rid of it. A premature baby may have trouble processing
bilirubin because its own liver is not ready to take over this
function. Full-term babies can also have this problem.
A newborn baby with high bilirubin may exhibit jaundice.
Jaundice in a newborn usually occurs when bilirubin being handled by
the mother’s system must now be handled by the baby it on its own. The
baby’s liver can’t keep up.
4. Changes in You
Fetal Fibronectin (fFN)
It can be hard to determine if a woman
is at risk of delivering a preterm baby. Many symptoms of preterm labor
are similar to various discomforts of pregnancy. A test is available
that can help healthcare providers.
Fetal fibronectin (fFN) is a protein
found in the amniotic sac and fetal membranes. However, after 22 weeks
of pregnancy, fFN is not normally present until around week 38.
When found in cervical-vaginal secretions
of a pregnant woman after 22 weeks (before week 38), it means there is
a higher risk for preterm delivery. If not found, risk of premature
labor is low, and the woman probably won’t deliver within the next 2
weeks. fFN can rule out early delivery with 99% accuracy.
The test is similar to a Pap
smear. A swab of vaginal secretions is taken from the top of the
vagina, behind the cervix. It is sent to the lab, and results are
available within 24 hours.
What Is Anemia?
There is a fine balance in your body
between the production of red blood cells that carry oxygen to the rest
of your body and the destruction of these cells. Anemia is the condition in which the number of red blood cells is low. If you’re anemic, you don’t have enough red blood cells.
By the 22nd week of pregnancy (fetal age—20 weeks),
your baby’s eyelids and eyebrows are well developed.
Fingernails now cover the fingertips.
During pregnancy, the number of red blood cells increases. The amount of plasma (liquid part of the blood) also increases but at a higher rate. Your healthcare provider keeps track of these changes with a hematocrit reading, a measure of the percentage of the blood that is red blood cells. This is usually done at the first prenatal visit.
If your temperature rises above 100F,
contact your healthcare provider. A temperature above 102F may indicate
an infection is bacterial.
Your hemoglobin level is also
tested. Hemoglobin is the protein component of red blood cells. If
you’re anemic, your hematocrit is lower than 37, and your hemoglobin is
under 12. The test may be repeated once or twice during pregnancy and
is done more often if you’re anemic. If you suffer from anemia during
pregnancy, you won’t feel well, you’ll tire easily and you may
experience dizziness. Treatment is important for you and your baby.
There is always some blood loss at
delivery. If you’re anemic when you go into labor, you may need a blood
transfusion after your baby is born.
Follow your healthcare provider’s advice
about diet and supplementation if you have anemia.
Iron-Deficiency Anemia. The most common type of anemia seen in pregnancy is iron-deficiency anemia.
During pregnancy, your baby uses some of the iron stores you have in
your body. If you have iron-deficiency anemia, your body doesn’t have
enough iron left to make red blood cells because the baby has used some
of your iron for its own blood-cell production. It’s important to treat
the problem. Iron deficiency has been tied to increased risks.
Most prenatal vitamins contain iron, but
it’s also available as a supplement. If you can’t take a prenatal
vitamin, you may be given 300 to 350mg of ferrous sulphate or ferrous
gluconate 2 or 3 times a day. Iron is the most important supplement to take during pregnancy and is required in almost all pregnancies.
Some women develop iron-deficiency anemia
during pregnancy even if they take iron supplements. Several factors
may make a woman more likely to have this condition in pregnancy,
including:
• bleeding during pregnancy
• multiple fetuses
• previous surgery on the stomach or part of the small bowel
• antacid overuse that causes a decrease in iron absorption
• poor eating habits
The goal in treating iron-deficiency
anemia is to increase the amount of iron you take in. Iron is poorly
absorbed so you need to take it every day. It can be given as an
injection, but it’s painful and may stain the skin.
Side effects of taking iron supplements
include nausea and vomiting, with stomach upset. If this occurs, you
may have to take a lower dose. Taking iron may also cause constipation.
If you can’t take an iron
supplement, eat more foods that are high in the mineral. Liver or
spinach are good choices. Ask your healthcare provider for information
on what types of foods you should include in your diet.