1. How Big Is Your Baby?
The fetal crown-to-rump length
by this week of pregnancy is 4 to 4½ inches (9.3 to 10.3cm). The fetus
weighs about 1¾ ounces (50g). It’s close to the size of a softball.
2. How Big Are You?
Changes in your lower abdomen
change the way your clothes fit. Your pregnancy may not be obvious to
other people when you wear regular clothes. But it may become obvious
if you start wearing maternity clothes or put on a swimming suit. You
may be able to feel your uterus about 3 or 4 inches (7.6 to 10cm) below
your belly button.
3. How Your Baby Is Growing and Developing
It’s still a little early to feel
movement, although you should feel your baby move in the next few
weeks! Your baby’s skin is thin, and you can see blood vessels through
the skin.
Your baby may be sucking its thumb. This has been seen with ultrasound examination.
Ears now look more normal. In fact, your baby looks more human every
day. Bones that have already formed are getting harder. If an X-ray
were done at this time, the baby’s skeleton would be visible.
4. Alpha-Fetoprotein (AFP) Testing
As baby grows, it produces alpha-fetoprotein
(AFP) in its liver and passes some of it into your bloodstream. It’s
possible to measure AFP by drawing your blood; too much or not enough
of the protein in your blood can be a sign of problems.
An AFP test is usually done between 16
and 18 weeks of gestation. Timing is important and must be tied to the
gestational age of your pregnancy and to your weight. An important use
of the test is to help a woman decide whether to have amniocentesis.
An elevated AFP level can indicate
problems in the baby. A connection has been found between a low level
of AFP and Down syndrome. If your AFP level is abnormal, your
healthcare provider may choose to do other tests to look for problems.
Tip for Week 15
Start now to learn to sleep on your
side; it will pay off later as you get bigger. Sometimes it helps to
use a few extra pillows. Put one behind you so if you roll onto your
back, you won’t lie flat. Put another pillow between your legs, or rest
your top leg on a pillow. Consider using a “pregnancy pillow” that
supports your entire body.
The AFP test is not done on all
pregnant women, although it is required in some states. It is not used
routinely in Canada. AFP is often used with other tests. If the test
isn’t offered to you, ask about it. There’s little risk, and it helps
your healthcare provider determine how baby is growing and developing.
5. Changes in You
During your first prenatal visit, you
probably had a Pap smear; one is usually done at the beginning of
pregnancy. By now, the result is back, and you’ve discussed it with
your healthcare provider, particularly if it was abnormal.
A Pap smear identifies cancerous or
precancerous cells coming from the cervix. This test has helped
decrease the number of deaths from cervical cancer because of early
detection and treatment.
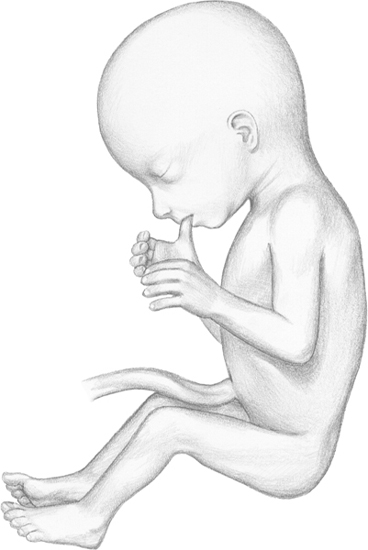
By week 15 of pregnancy (fetal age—13 weeks),
your baby may suck its thumb. Eyes are at the front of
the face but are still widely separated.
An abnormal Pap
smear during pregnancy must be handled individually. When abnormal
cells are “not too bad” (premalignant or not as serious), it may be
possible to watch them during pregnancy.
If your healthcare provider is concerned, he or she may do a colposcopy,
a procedure to examine the cervix. Abnormal areas can be seen so
biopsies can be taken after pregnancy. Most obstetricians/gynecologists
can do this procedure in the office.
There are several ways to treat abnormal
cells on the cervix, but most treatment methods aren’t done during
pregnancy. After pregnancy, the problem will be revisited.
Women who deliver vaginally may see a
change in abnormal Pap smears. One study showed over half of the women
who had problems before giving birth had normal Pap smears after their
baby was born.