1. How Big Is Your Baby?
By this week, baby weighs about 1¼ pounds (540g). Its crown-to-rump length is about 8½ inches (21cm).
2. How Big Are You?
Your uterus is now about 1½ to 2
inches (3.8 to 5.1cm) above the bellybutton. It measures almost 10
inches (24cm) above the pubic symphysis.
3. How Your Baby Is Growing and Developing
Your baby is filling out. Its face and
body look more like that of an infant at the time of birth. Although it
weighs a little over 1 pound at this point, it is still very tiny.
The baby grows in amniotic fluid inside the amniotic sac. Amniotic fluid has several important functions. It provides an
environment in which the baby can move easily and cushions the fetus
against injury. It regulates temperature. It also provides a way of
assessing the health and maturity of the baby.
Amniotic fluid increases rapidly from an
average volume of 1½ ounces (50ml) by 12 weeks of pregnancy to 12
ounces (400ml) at midpregnancy. The volume of amniotic fluid continues
to increase as your due date approaches until a maximum of about 2
pints (1 liter) of fluid is reached at 36 to 38 weeks gestation.
Makeup of amniotic
fluid changes during pregnancy. During the first half of pregnancy,
it’s similar to the fluid in your blood without blood cells, except it
has a much lower protein content. As baby grows, fetal urine adds to
the amount of amniotic fluid present. Amniotic fluid also contains old
fetal blood cells, lanugo hair and vernix.
The fetus swallows amniotic
fluid during much of pregnancy. If it can’t swallow the fluid, you may
develop a condition of excess amniotic fluid, called hydramnios or polyhydramnios.
If the fetus swallows but doesn’t urinate (for example, if the baby
lacks kidneys), the volume of amniotic fluid surrounding the fetus may
be very small. This is called oligohydramnios.
4. Changes in You
Nasal Problems
Some women complain of stuffiness in
their nose or frequent nosebleeds during pregnancy. Some experts
believe these symptoms occur because of circulation changes caused by
hormonal changes during pregnancy. Mucous membranes of your nose and
nasal passageways swell and bleed more easily.
A few decongestants and nasal sprays can
be used during pregnancy. Some brands to consider include
chlorpheniramine (Chlor-Trimeton) decongestants and oxymetazoline
(Afrin, Dristan Long-Lasting) nasal sprays. Before you begin using any
product, discuss it with your healthcare provider.
It may also help to use a
humidifier, particularly during winter months when heating may dry out
the air. Some women get relief from increasing their fluid intake
and/or using a gentle lubricant in their nose, such as petroleum jelly.
Depression
Depression can occur at any time during
a person’s life. Many things can contribute to depression, including
chemical imbalances in the body, stressful life events and situations
that cause anxiety and tension. If you have a history of major
depression, you’re at increased risk of depression occurring during
pregnancy. In fact, between 3 and 5% of all women experience a major
depression during pregnancy. It’s estimated another 15% have some
degree of depression.
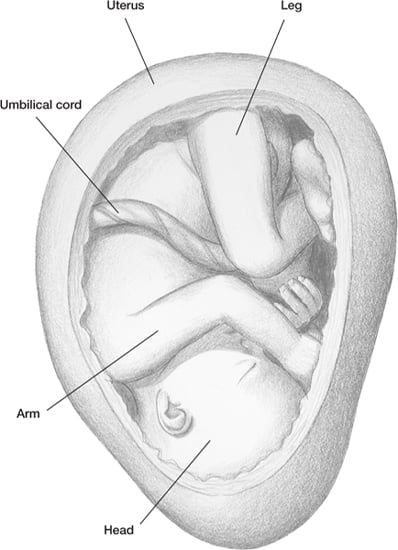
The fetus doesn’t appear to have a great deal of
room to move in the uterus by the 24th week.
As the weeks pass, space gets even tight
If you’re being
treated for depression when you get pregnant, it’s important to
continue treatment. Treating depression is as important as treating any
other problem.
If you take antidepressants, don’t stop
unless advised by your healthcare provider to do so. Studies show up to
70% of women who stop taking antidepressants during pregnancy relapse
into depression. Stopping your medication can raise stress hormones,
which increases your risks of problems during pregnancy. The risks to
you and your baby from depression may be greater than your risk of
taking antidepressants. We know depression can be difficult to manage
without using drug therapy.
There may be a very small increased risk
of birth defects with some medicines used to treat depression when
taken during the first trimester. It may help to switch to an
antidepressant that is safer during pregnancy, including fluoxetine
(Prozac), citalopram and escitalopram (Lexapro). Pregnancy may affect
your body’s ability to use lithium. If you take an SSRI, the dose may
need to be increased during the third trimester to maintain your normal
mood. Talk to your healthcare provider as soon as you confirm your
pregnancy.
There is continued concern about the
safety of Paxil during pregnancy. Research suggests using the drug in
the first trimester of pregnancy may be tied to an increased risk of
heart problems in baby. However, do not stop taking your antidepressant medicine without first consulting your healthcare provider.
If you’re feeling depressed, your level
of vitamin D may be low. Talk about it with your healthcare provider.
Other suggestions for dealing with depression include getting some
exercise and being sure you get enough B vitamins, folic acid and
omega-3 fatty acids. Taking about 3.5g of omega-3 fatty acids every day
has been shown to help fight depression.
Additional therapies include massage and
reflexology. Another option is light therapy, similar to the type of
treatment given to those who suffer from “seasonal affective disorder.”
Depression during Pregnancy. Depression during
pregnancy does occur. Experts believe it’s one of the most common
medical problems seen in pregnant women. Studies show up to 25% of all
moms-to-be experience some degree of depression, and nearly 10% will
experience a major depression. And if left untreated, 50% of women who
are depressed during pregnancy will experience postpartum depression.
Treating depression during pregnancy is
important for your health and baby’s health. This is one of the many
reasons healthcare providers today make treating depression a priority.
Dad Tip
Now’s a good time to explore prenatal
classes in your area. Encourage your partner to find out how many
classes there are, when and where to register, and the registration
cost. You may be able to take classes at the hospital or birthing
center where your partner plans to deliver. Try to complete the classes
at least 1 month before baby is due.
Depression is actually more common during
pregnancy than after giving birth.
If you have a family history of depression, you may be at higher risk
during pregnancy. If you don’t have enough serotonin, researchers
believe you may be at higher risk. If you’ve been struggling with
infertility or miscarriage, you may also be more prone to depression.
If you’re depressed, you may not take
good care of yourself. Babies born to depressed women may be smaller or
born prematurely. Some women use alcohol, drugs and cigarettes in an
attempt to ease their depression. You may also have trouble bonding
with your baby after birth.
Consider the following to measure your risks of being depressed. You may be at higher risk if:
• you experienced mood changes when you took oral contraceptives
• your mother was depressed during pregnancy
• you have a history of depression
• you feel sad or depressed longer than 1 week
• you’re not getting enough sleep and rest
• you have bipolar disorder—pregnancy can trigger a relapse, especially if you stop taking your mood-stabilizing medications
Symptoms and Treatment.
It may be hard to differentiate between some of the normal pregnancy
changes and signs of depression. Many symptoms of depression are
similar to those of pregnancy, including fatigue and sleeplessness. The
difference is how intense the symptoms are and how long they last. Some
common symptoms of depression include:
• overpowering sadness that lasts for days, without an obvious cause
• difficulty sleeping, or waking up very early
• wanting to sleep all the time or
great fatigue (this can be normal early in pregnancy but usually gets
better after a few weeks)
• no appetite (as distinguished from nausea and vomiting)
• lack of concentration
• thoughts of harming yourself
Women who are depressed are more likely
to develop diabetes, and women who develop diabetes are more likely to
be depressed. This is also true for pregnant women. If you have
diabetes and untreated depression, then become pregnant, it can be
serious if you don’t get help. You may have a difficult time caring for
yourself. This could lead to difficulties in controlling weight and
sugar levels. Your risk of addictive-substance abuse, such as alcohol
use and cigarette smoking, may increase. And you may not be able to
meet the nutritional demands of your pregnancy.
Research shows it’s better for baby if only one medicine is used during pregnancy to treat a woman’s depression.
Babies born to mothers with untreated
depression can have many problems. They often cry a lot, have
difficulty sleeping, are fussier and are difficult to soothe.
If you have symptoms and they
don’t get better in a few weeks or every day seems to be bad, seek help
as soon as you recognize you might be depressed. Call your healthcare
provider, or bring it up at your next prenatal visit. There are steps
to take to help you feel better again. It’s important to do it for
yourself and your baby!