Most women plan on a vaginal birth, but
a Cesarean delivery is always a possibility. With a Cesarean, the baby
is delivered through an incision made in the mother’s abdominal wall
and uterus. An emergency Cesarean delivery is one that is unplanned. An elective Cesarean delivery is planned and done without a medical reason.
The main advantage to having a Cesarean
delivery is delivery of a healthy infant. A Cesarean may be the safest
way for your baby to be born. The disadvantage is Cesarean delivery is
a major operation and carries with it all the risks of surgery.
It would be nice to know you’re going to
need a Cesarean so you wouldn’t have to go through labor.
Unfortunately, you don’t know ahead of time if you will have problems.
Some women believe if they have a
Cesarean, “it won’t be like having a baby.” They falsely believe they
won’t experience the birth process. That’s not true. If you have a
Cesarean delivery, try not to feel this way. You haven’t failed in any
way!
It may be difficult at times to tell the
exact location of different parts of the baby. You may have a good idea
according to where you feel kicks and punches. Ask your doctor to show
you on your tummy how the baby is lying. Some doctors will take a
marking pen and draw on your stomach to show you how baby is lying. You
can leave it so you can later show your partner how baby was lying when
you were seen in the office that day.
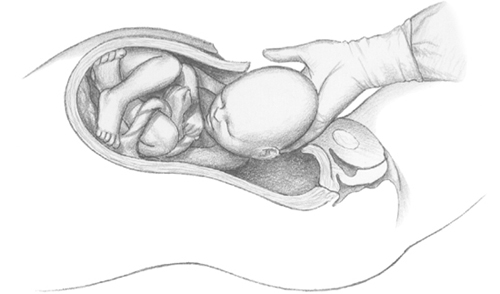
Delivery of a baby by Cesarean section.
Remember, having a baby has taken 9 long months. Even with a Cesarean delivery, you have accomplished an amazing feat.
Reasons for Cesareans.
Cesareans are done for many reasons. They are often performed when
there’s a problem during labor. The most common reason for having one
is a previous Cesarean delivery. Nine out of 10 women who have had a
previous Cesarean delivery choose a repeat Cesarean for the next birth.
Some women who have had Cesareans may be able to have a vaginal delivery with later pregnancies; this is called vaginal birth after Cesarean (VBAC).
Nonmedical factors for having a Cesarean
include maternal choice, more conservative practice guidelines and
legal pressures. If you’re exhausted when you begin labor, you may also
be at a higher risk for a Cesarean section. Pre-eclampsia or an active
herpes sore may require a Cesarean delivery.
A Cesarean may be necessary if your baby is too big to fit through the birth canal, called cephalo-pelvic disproportion (CPD).
CPD may be suspected during pregnancy, but usually labor must begin
before it can be confirmed. A Cesarean may be recommended if an
ultrasound shows your baby is very large—9½ pounds or larger—and may
not be easily delivered vaginally.
Fetal stress is an important reason a
Cesarean delivery may be performed. The fetal heartbeat and its
response to labor is often monitored. If the heartbeat indicates baby
is having trouble with labor contractions, a Cesarean may be necessary.
It’s possible for you to dilate during
labor without the baby moving down through the pelvis. When baby’s head
is too large to fit through the birth canal, it results in failure to progress. This situation is one of the most common reasons for a Cesarean delivery.
If the umbilical cord is compressed, a
Cesarean may be necessary. The cord may come into the vagina ahead of
the baby’s head or the baby can press on part of the cord. This is a dangerous because a compressed cord can cut off baby’s blood supply.
A Cesarean may be needed if you’re older.
The Cesarean-delivery rate for mothers between 40 and 54 years old is
more than double the rate for women younger than age 20.
A Cesarean is often necessary if baby is
in a breech presentation, which means baby’s feet or buttocks enter the
birth canal first. Delivering the shoulders and the head after baby’s
body may damage the baby’s head or neck, especially with a first baby.
Placental abruption or placenta previa
are also reasons for a Cesarean delivery. If the placenta separates
from the uterus before delivery (placental abruption), the baby loses
its supply of oxygen and nutrients. This is usually diagnosed when a
woman has heavy vaginal bleeding. If the placenta blocks the birth
canal (placenta previa), the baby can’t be delivered any other way.
A Cesarean delivery for a first baby
increases a woman’s chances for placenta previa or placental abruption
in her next pregnancies. A repeat Cesarean increases a woman’s risk of
placenta accreta in subsequent pregnancies if the placenta implants low
in the uterus and grows into the area of the previous Cesarean-delivery
incision.
If complications arise during pregnancy
or while you’re in labor, your CNM, NP or PA will consult a physician
specializing in pregnancy.
Rising Rate of Cesarean Deliveries.
In 1965, only 4% of all deliveries were by C-section. Between 1996 and
2007, there was a 71% increase in Cesarean births. In 2007, 32% of all
live births in the United States were Cesarean deliveries (more than
1.2 million); in 2008 that number rose to 32.3%. Today in the United
States, Cesarean deliveries account for over 30% of all deliveries. In
some areas, this percentage is even higher.
The rising rate is related in part to
closer monitoring during labor and safer procedures for Cesarean
deliveries. Part of the increase can also be attributed to the increase
in multiple births, but the Cesarean rate actually increased more for
singletons than for multiples.
Babies delivered by
a scheduled Cesarean delivery between 37 and 39 weeks have more
respiratory problems than babies born vaginally or by emergency
Cesarean at the same point in pregnancy. It’s believed hormones
released during labor help baby deal with fluid in the lungs. The
compressions of the baby’s chest from labor are also believed to help
clear amniotic fluid from baby’s lungs.
Elective Cesarean Deliveries. Part of the increase in Cesarean deliveries in the United States is due to Cesarean delivery on maternal request (CDMR). It is also called patient-requested Cesarean.
There are many reasons for choosing a
Cesarean delivery, including fear of labor, concern over vaginal
tearing and worry about incontinence later. Some women believe a
Cesarean will help them retain their prepregnancy figure; however it’s
pregnancy, not giving birth, that stretches the waistline. Other women
believe a Cesarean is safer for baby.
In some parts of the world, elective
Cesarean delivery is not a big issue. In many Latin American countries,
the rate of elective Cesareans is 40 to 50%. One survey conducted in
Brazil showed private hospitals, where the wealthiest patients go, had
an 80 to 90% rate of elective Cesareans.
U.S. doctors are split on the question of
elective Cesarean delivery. There’s evidence supporting both sides.
Some believe with improved anesthesia, antibiotics, infection control
and pain management, a Cesarean is no riskier than vaginal delivery.
However, ACOG, the federal government, the American College of
Nurse-Midwives and Lamaze International believe we should look more
closely at the present Cesarean-delivery rate.
The point in pregnancy when a Cesarean is
scheduled is also important. It’s amazing how much difference a few
days can make to the health of your baby. The latest recommendations
are that a woman not schedule a Cesarean delivery any earlier
than 39 weeks, unless tests show the baby’s lungs are mature. Research
shows a baby will do better if he or she is born within 7 days of its
due date. If a baby is delivered earlier than
this, he or she may have more problems. When compared with babies
delivered at 37 or 38 weeks, those born at 39 weeks or more had
significantly lower rates of problems.
How Is a Cesarean Delivery Performed?
If problems arise during pregnancy and/or labor, if your care has been
provided by a CNM, PA or NP, he or she may consult a physician. In most
areas, an obstetrician performs a Cesarean. In small communities, a
general surgeon or a family practitioner may perform Cesarean
deliveries.
If you’re scheduled to have a Cesarean,
follow directions for eating before surgery. You are often awake when a
Cesarean is done. If you are, you may be able to see your baby
immediately after delivery!
You’re first visited by the
anesthesiologist to discuss pain-relief methods. Up to 90% of all
elective Cesarean deliveries are done with spinal anesthesia.
After you receive anesthesia, your doctor
begins by making a 5- to 6-inch incision in the area above your pubic
bone. A cut is made through tissue down to the uterus, where a
horizontal incision is made into the lower part of the uterus. After
all the incisions are made, the doctor reaches into the uterus and
removes the baby, then the placenta. Each layer is sewn together with
absorbable sutures; the entire procedure takes 30 minutes to an hour.
In the past, a Cesarean was often done
with a classical incision, in which the uterus was cut down the
midline. This incision doesn’t heal as well because it is made in the
muscular part of the uterus. It’s more likely to pull apart with
contractions (as in a vaginal birth after Cesarean). This can cause
heavy bleeding and injure the baby. If you have had a classical
Cesarean section in the past, you must have a Cesarean delivery every time you have a baby.
Today, most Cesarean deliveries are low-cervical Cesareans or low-transverse
Cesareans. This means the incision is made low in the uterus. Or a
T-incision may be used. It goes across and up the uterus in the shape
of an inverted T. It provides more room to get baby out. If you have a
T-incision, you may need a Cesarean delivery with all subsequent
pregnancies because it may be more likely to rupture.
After Your Cesarean Delivery. If you’re awake for baby’s birth, you may be able to hold him or her immediately. You may also have a chance to begin nursing.
You may need pain relief for the incision. One device to help deal with the pain after a Cesarean is ON-Q. A small catheter is inserted underneath the skin, which sends a local painkiller to the incision
area of the Cesarean so very little, if any, medication gets to baby
through your breast milk. Studies show moms who receive ON-Q after a
Cesarean are able to get out of bed and walk around more quickly, and
their hospital stays are shorter. Ask your doctor about it at one of
your prenatal visits.
You’ll probably stay in the hospital 2 to
4 days. Recovery at home from a Cesarean delivery takes longer than
recovery from a vaginal delivery. The normal time for full recovery is
usually 4 to 6 weeks.