6. Your Nutrition
Salmonella poisoning can negatively impact a pregnancy. Salmonella bacteria can cause a lot of problems for you. Any could be serious.
Salmonella bacteria has many
sources—there are over 1400 different strains! They’re found in raw
eggs and raw poultry. The bacteria is destroyed when a food is cooked,
but it’s wise to take additional precautions. Keep in mind the
following measures to stay safe.
• Clean your counters, utensils, dishes and pans with hot water and soap or a disinfecting agent when you clean up.
• Cook poultry thoroughly.
• Don’t eat products made with raw
eggs, such as Caesar salad, hollandaise sauce, homemade eggnog,
homemade ice cream and so on. Don’t taste cake batter, cookie dough or
anything else that contains raw eggs before it’s cooked.
•
When you eat eggs, be sure they’re cooked thoroughly. Boil eggs for at
least 7 minutes. Poach eggs for 5 minutes. Fry them on each side for 3
minutes—cook them so the yolk and white are firm. Don’t eat “sunnyside
up” eggs.
7. You Should Also Know
Carpal Tunnel Syndrome during Pregnancy
If you have carpal tunnel syndrome, you
have pain in the hand and wrist, which can extend into the forearm and
shoulder. It’s caused when the median nerve in the wrist is squeezed by
swelling in the wrist and arm area. Symptoms can be numbness, tingling
or burning of the inner half of one or both hands. At the same time,
fingers feel numb and useless. More than half of the time, both hands
are involved.
Pineapple contains brome-lain, an enzyme
that helps ease swelling, inflammation and bruising. Consider adding
some to your meal plan.
Up to 25% of all pregnant women
experience mild symptoms, but treatment is usually unnecessary. The
full syndrome, in which treatment may be needed, is less frequent; it
occurs in only 1 to 2% of pregnant women.
Treatment depends on symptoms. In
pregnant women, splints are often used during sleep and rest to try to
keep the wrist straight. Symptoms usually disappear after delivery.
Occurrence of carpal tunnel syndrome during pregnancy does not
mean you’ll suffer from it after baby’s birth. In rare instances,
symptoms may recur long after pregnancy. In these cases, surgery may be
necessary.
Pregnancy-Induced Hypertension (PIH)
When high blood pressure occurs only during pregnancy, it is called pregnancy-induced hypertension (PIH) or gestational hypertension. The problem usually disappears after baby is born.
With PIH, the systolic pressure (the
first number) increases to higher than 140ml of mercury or a rise of
30ml of mercury over your beginning blood
pressure. A diastolic reading (the second number) of over 90ml or a
rise of 15ml of mercury also indicates a problem. An example is a woman
whose blood pressure at the beginning of pregnancy is 100/60. Later in
pregnancy, it is 130/90. This signals she may be developing high blood
pressure or pre-eclampsia.
If pizza has been left out on the
counter for over 2 hours, throw it out. Bacteria can grow on the cheese
and toppings, and cause food poisoning. If you want to keep leftover
pizza, refrigerate it in an airtight plastic container immediately
after you’re finished eating.
We have seen some articles in magazines and newspapers that incorrectly equate high blood pressure with pre-eclampsia. They are not the same problem. High blood pressure is one common sign
of pre-eclampsia, but it must be accompanied by other serious symptoms
for you to be diagnosed with pre-eclampsia. See the discussion below.
Be sure to follow your healthcare provider’s advice about taking care
of high blood pressure, but don’t panic.
Your healthcare provider will be
able to determine if your blood pressure is rising to a serious level
by checking it at every prenatal appointment. That’s one of the reasons
it’s so important to keep all your prenatal appointments.
What Is Pre-eclampsia?
Pre-eclampsia describes a group of symptoms that occur only
during pregnancy or shortly after delivery. Pre-eclampsia seems to be
on the rise; the condition affects 1 in 20 pregnancies and accounts for
over 15% of all maternal deaths during pregnancy.
No one knows what causes pre-eclampsia
(or eclampsia). It occurs most often during a woman’s first pregnancy.
Women over 35 years old who are having their first baby are more likely
to develop high blood pressure and pre-eclampsia. Some experts believe job stress may be a contributing factor. If you’re in a stressful job situation, discuss it with your healthcare provider.
Pre-eclampsia occurs more often in women
who have had chronic high blood pressure and pre-eclampsia in a
previous pregnancy. Keeping a close watch on you throughout pregnancy
and checking your blood pressure and weight at every prenatal visit can alert your healthcare provider to a developing problem.
Pre-eclampsia problems are characterized by a collection of symptoms. The first four are the most common:
• swelling (edema)
• protein in the urine (proteinuria)
• high blood pressure (hypertension)
• a change in reflexes (hyperreflexia)
• swelling and pain in a foot may worsen
• rapid weight gain, such as 10 to 12 pounds in 5 days
• flulike aches and pain, without a runny nose or sore throat
• headaches
• vision changes or problems
• elevated level of uric acid
• pain under the ribs on the right side
• seeing spots
Report symptoms to your healthcare provider immediately, particularly if you’ve had blood-pressure problems during pregnancy!
Most pregnant women have some swelling during pregnancy. Swelling in the legs and/or hands does not mean you have pre-eclampsia.
Weight gain can be a sign of a developing
problem. Pre-eclampsia increases water retention, which can increase
your weight. If you notice an unusual, rapid weight gain, contact your
healthcare provider.
Risk factors for developing pre-eclampsia include the following:
• history of high blood pressure before pregnancy
• kidney disease
• thrombophilia (blood-clotting disorders)
• some autoimmune disorders
• younger than 20 years old
• delaying childbirth until after age 35
• overweight or obesity
• multiple fetuses
• diabetes or kidney disease
• Black/African American ethnicity
Taking a
multivitamin regularly before getting pregnant may help reduce your
risk of pre-eclampsia. Eating high-fiber foods during the first
trimester may also help reduce risks. Garlic has been shown to help
reduce risks. Even eating five servings a week of dark chocolate may reduce your risk. Ask your healthcare provider his or her opinion, if you have questions.
Controlling asthma during pregnancy may
help lower your risk of developing pre-eclampsia. Talk to your
healthcare provider if you have questions.
A father-to-be’s age may play a role in
pre-eclampsia. One study showed the problem is 80% higher among women
whose partners are 45 years or older.
There are ways to help lower your risk of
developing pre-eclampsia. Get regular exercise. Take care of your teeth
so you don’t get gum disease. Take folic acid. Eat foods high in fiber.
Some researchers believe if a woman has
pre-eclampsia, her blood vessels may never have properly dilated from
the beginning of pregnancy.
Treating Pre-eclampsia. Pre-eclampsia can progress to eclampsia—seizures
or convulsions in a woman with pre-eclampsia. The goal in treating
pre-eclampsia is to avoid eclampsia. Seizures are not caused by a
previous history of epilepsy or a seizure disorder.
Some experts believe low-dose-aspirin
therapy may help prevent preeclampsia. The crucial time to begin taking
it is around 12 weeks of pregnancy. Talk to your healthcare provider
about it if you had pre-eclampsia with a previous pregnancy.
Treatment begins with bed rest at home.
You may not be able to work or to spend much time on your feet. Bed
rest provides the greatest blood flow to the uterus.
Lie on your side, not on your back. Drink
lots of water. Avoid salt, salty foods and foods that contain sodium,
which may make you retain fluid. Diuretics are not prescribed to treat
pre-eclampsia and are not recommended. If a woman with pre-eclampsia
has a systolic blood-pressure reading of 155 to 160ml, she should be
treated with antihy-pertensive therapy to help prevent a stroke.
If you can’t rest at
home in bed or if symptoms don’t improve, you may be admitted to the
hospital or your baby may need to be delivered. A baby is delivered for
its well-being and to avoid seizures in you.
During labor, pre-eclampsia may be
treated with magnesium sulfate. It is given by I.V. to prevent seizures
during and after delivery.
If you think you’ve had a
seizure, call your healthcare provider immediately! Diagnosis may be
difficult. If possible, someone who saw the possible seizure should
describe it to your healthcare provider. Eclampsia is treated with
medications similar to those prescribed for seizure disorders.
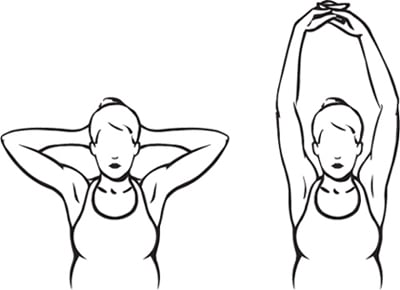
8. Exercise for Week 31
Sit up straight in a chair or on the
floor. Lace your fingers together behind your head; keep your elbows
apart. Inhale and push your hands, with your fingers still together,
toward the ceiling. Exhale and return your hands to the position behind
your head. Repeat 5 times. Tones arms and shoulder muscles.