Sickle-Cell Disease
Sickle-cell disease is the most common
hemoglobin disorder in the United States. About 8% of Black/African
Americans carry the sickle-hemoglobin gene. However, it is also found
in people of Arabic, Greek, Maltese, Italian, Sardinian, Turkish,
Indian, Caribbean, Latin American and Middle-Eastern descent. In the
United States, most cases of sickle-cell disease occur among
Black/African Americans and Latino/Hispanics. About one in every 500
Black/African Americans has sickle-cell disease.
Sickle-cell disease is inherited.
Normally, red blood cells are round and flexible, and flow easily
through blood vessels. In sickle-cell disease, abnormal hemoglobin
causes red blood cells to become stiff. Under the microscope, they may
look like the C-shaped farm tool called a sickle.
Because they are stiffer, these red blood
cells can get stuck in tiny blood vessels and cut off the blood supply
to nearby tissues. This causes a great deal of pain (called sickle-cell pain episode or sickle-cell crisis)
and may damage organs. These abnormal red blood cells die and break
down more quickly than normal red blood cells, which results in anemia.
A person who inherits the sickle-cell
gene from one parent and the normal type of that gene from the other
parent is said to have sickle-cell trait. Carriers of the
sickle-cell gene are usually as healthy as non-carriers. Sickle-cell
trait cannot change to become sickle-cell disease.
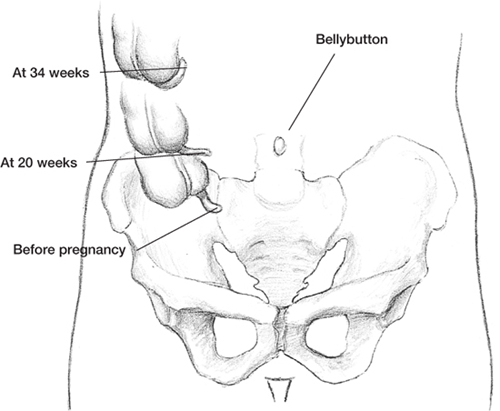
Location of the appendix at various times during pregnancy.
When two people with
sickle-cell trait have a child, there is a one-in-four chance their
child may inherit two sickle-cell genes (one gene from each parent) and
have the disorder. There is a two-in-four chance the child will have
the trait. There is a one-in-four chance the child will have neither
the trait nor the disease. These chances are the same in each
pregnancy. If only one parent has the trait and the other doesn’t,
there is no chance their children will have sickle-cell disease. However, there is a 50–50 chance of each child having the trait.
Tip for Week 22
Drink extra fluids (water is best)
throughout pregnancy to help your body keep up with the increase in
your blood volume. You’ll know you’re drinking enough fluid when your
urine looks almost like clear water.
Sickle-cell disease can also affect
biracial children. To what degree depends on the ethnic group of each
parent and his or her genetic makeup. A union of a Caucasian and a
Black/African American will not result in a child with sickle-cell
disease because Caucasians are not carriers of the sickle-cell gene.
However, the union of a Black/ African American and a person of
Mediterranean or Latino/Hispanic descent could result in a
child with sickle-cell disease if both parents carry the sickle-cell
gene. In addition, if both parents are biracial, they could pass the
disease to their children if each parent carries the gene. The risk of
both biracial partners being carriers is lower, but the risk is still
there and depends on each person’s genetic background and makeup.
Pregnancy and Sickle-Cell Disease.
A woman with sickle-cell disease can have a safe pregnancy. However, if
you have the disease, your chances are greater of having problems that
can affect your health and your baby’s health.
During pregnancy, the disease may become
more severe, and pain episodes may be more frequent. You will need
early prenatal care and careful monitoring throughout pregnancy.
Until 1995, there was no effective
treatment, other than blood transfusions, to prevent the sickling of
the blood that causes a pain crisis. The medication, hydroxyurea, was
found to reduce the number of pain episodes by
about 50% in some severely affected adults. At this time, we do not
recommend hydroxyurea for pregnant women. However, researchers continue
to study new drug treatments to help reduce complications of the
disease.
A blood test can reveal sickle-cell
trait. There also are prenatal tests to find out if a baby will have
the disease or carry the trait. Most children with sickle-cell disease
are now identified through newborn screening tests.
Your healthcare provider will pay close
attention to your sickle-cell disease during pregnancy. Work with your
healthcare team to stay as healthy as possible.
Thalassemia
Thalassemia, also called Cooley’s anemia,
is not just one disease. It includes a number of different forms of
anemia. The thalassemia trait is found all over the world but is most
common in people from the Middle East, Greece, Italy, Georgia (the
country, not the state), Armenia, Viet Nam, Laos, Thailand, Singapore,
the Philippines, Cambodia, Malaysia, Burma, Indonesia, China, East
India, Africa and Azerbaijan. It affects about 100,000 babies each year.
There are two main forms of the
disease—alpha thalassemia and beta thalassemia. The type depends on
which part of an oxygen-carrying protein (the hemoglobin) is lacking in
red blood cells. Most individuals have a mild form of the disease. The
effects of beta thalassemia can range from no effects to very severe.
Eating Dark Chocolate
Eating dark chocolate (at least 70%
cocoa content) may be good for you. A daily dose of 30g of dark
chocolate has been associated with lower blood pressure and a reduced
risk of anemia. Chocolate also helps relax and dilate blood vessels to
help lower blood pressure. Antioxidants found in dark chocolate may be
healthy for you. Keep in mind the following when choosing dark
chocolate.
• Chocolate should be 70% or more cocoa.
• Don’t eat more than 3 ounces a day.
• Dark chocolate should replace other sweets.
A carrier of thalassemia has one normal gene and one thalassemia gene; this is called the thalassemia trait. Most carriers lead completely normal, healthy lives.
When two carriers have a child, there is
a one-in-four chance their child will have a form of the disease. There
is a two-in-four chance the child will be a carrier like its parents
and a one-in-four chance the child will be completely free of the
disease. These odds are the same for each pregnancy when both parents
are carriers.
Various tests can determine whether a
person has thalassemia or is a carrier. Chorionic villus sampling (CVS)
and amniocentesis can detect thalassemia in a fetus. Early diagnosis is
important so treatment can begin at birth to prevent as many
complications as possible.
Having the thalassemia trait doesn’t
usually cause health problems, although women with the trait may be
more likely to develop anemia during pregnancy. Healthcare providers
may treat this with folic-acid supplementation.
Most children born with thalassemia
appear healthy at birth, but during the first or second year of life
they develop problems. They grow slowly and often develop jaundice.
Treatment of thalassemia includes
frequent blood transfusions and antibiotics. When children are treated
with transfusions to keep their hemoglobin level near normal, many
complications of thalassemia can be prevented. However, repeated blood
transfusions may lead to a buildup of iron in the body. A drug called
an iron chelator may be given to help rid the body of excess iron.
Certified Nurse-Midwives, Advance-Practice Nurses and Physician Assistants
In today’s obstetric-and-gynecology
medical practices, you may find many types of highly qualified people
helping to take care of you. These people—mostly women, but not
all!—are on the forefront in guiding women through pregnancy to
delivery. They may even help deliver their babies!
A certified nurse-midwife (CNM)
is an advance-practice registered nurse (RN). He or she has received
additional training delivering babies and providing prenatal and
postpartum care to women. A CNM works closely with a doctor or team of
doctors to address specifics about a particular pregnancy, and labor
and delivery. Often a CNM delivers babies.
A certified midwife can provide many
types of information to a pregnant woman, such as guidance with
nutrition and exercise, ways to deal with pregnancy discomforts, tips
for managing weight gain, dealing with various pregnancy problems and
discussions of different methods of pain relief for labor and delivery.
A CNM can also address issues of family planning and birth control and
other gynecological care, including breast exams, Pap smears and other
screenings. A CNM can prescribe medications; each state has their own
specific requirements.
A nurse practitioner is also an
advance-practice registered nurse (RN). He or she has received
additional training providing prenatal and postpartum care to women. A
nurse practitioner may work with a doctor or work independently to
address specifics about a woman’s pregnancy, and labor and delivery.
A nurse practitioner can provide many
types of information to a pregnant woman, such as guidance with
nutrition and exercise, ways to deal with pregnancy discomforts, tips
for managing weight gain, dealing with various pregnancy problems and
discussions of different methods of pain relief for labor and delivery.
He or she can also address issues of family planning and birth control
and other gynecological care, including breast exams, Pap smears and
other screenings. In some cases, a nurse practitioner may prescribe
medications or provide pain relief during labor and delivery (as a
certified registered nurse anesthetist [CRNA]).
A physician assistant (PA)
is a qualified healthcare professional who may take care of you during
pregnancy. He or she is licensed to practice medicine in association
with a licensed doctor. In a normal, uncomplicated pregnancy, many or
most of your prenatal visits may be with a PA, not the doctor. This may
include labor and delivery. Most women find this is a good thing—often
these healthcare providers have more time to spend with you answering
questions and addressing your concerns.
A PA’s focus is to
provide many health-care services traditionally done by a doctor. They
care for people who have conditions (pregnancy is a condition they see
women for), diagnose and treat illnesses, order and interpret tests,
counsel on preventive health care, perform some procedures, assist in
surgery, write prescriptions and do physical exams. A PA is not a medical assistant, who performs administrative or simple clinical tasks.
We are fortunate to have these
dedicated professionals working in OB/GYN practices and clinics. The
care they provide is crucial to the medical community and makes quality
medical care for women something every woman can look forward to.
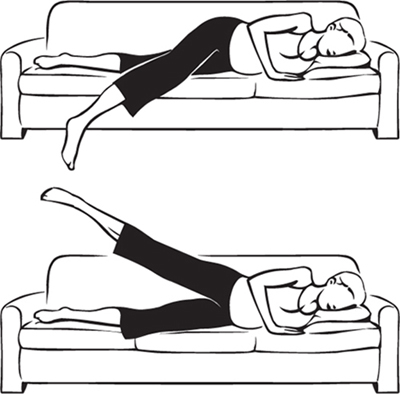
7. Exercise for Week 22
Lie on your left side on the sofa, with
your left knee bent. Bend your left arm, and place it under your head.
Lower your right foot to the floor while keeping your leg straight.
Hold for 10 seconds, then lift the straightened leg to a 45° angle;
hold for 5 seconds. Do 5 complete repetitions with each leg. Helps ease sciatica; strengthens hips and upper buttocks muscles.