Thyroid Disease
The thyroid gland produces
hormones to regulate metabolism and control functions in many of your
body’s organs. About 2% of all pregnant women have a thyroid disorder.
In fact, even if you don’t have a thyroid problem before pregnancy, if
there is a chance you could have a problem, it may appear during
pregnancy.
If you have a history of thyroid
problems, if you’re now taking medication or if you’ve taken medication
in the past, tell your healthcare provider. Discuss treatment during
pregnancy.
Left untreated, thyroid disorders can be
harmful to you and baby. Research shows women with a history of
miscarriage or premature delivery, or those who have problems near
delivery, may have problems with their thyroid-hormone levels.
You can go to parties while you’re
pregnant and still have a good time. A couple of things to remember—eat
something before you go and practice portion control.
Thyroid hormone is made in the thyroid
gland; this hormone affects your entire body and is important in
metabolism. Levels may be high or low. Low levels of thyroid cause a
condition called hypothyroidism; high levels cause hyperthyroidism.
Hypothyroidism is common during
pregnancy. Symptoms include unusual weight gain and fatigue (both of
which can be hard to determine during pregnancy), a hoarse voice, dry
skin, dry hair and a slow pulse. If you have these symptoms, tell your healthcare provider.
Hypothyroidism can affect your baby’s
health if you’re not treated. Your baby may not receive adequate
nutrition from you. Even with treatment, a baby is at risk of being
born with abnormal thyroid levels. Many weigh less than babies born to
mothers who didn’t have hypothyroidism.
Flavors from foods eaten by a mom-to-be pass into amniotic fluid, which may promote flavor preferences before
birth. By this time, baby can distinguish between sour, bitter and
sweet. We know even unborn babies have a natural preference for sweet.
Symptoms and Treatment.
Symptoms of thyroid disease may be masked by pregnancy. Or you may
notice changes during pregnancy that cause your healthcare provider to
suspect the thyroid is not functioning properly. These changes could
include an enlarged thyroid, changes in your pulse, redness of the
palms and warm, moist palms. Because thyroid-hormone levels can change
during pregnancy because of pregnancy, your healthcare provider must be careful interpreting lab results about this hormone while you’re pregnant.
The thyroid is tested primarily by blood
tests (a thyroid panel), which measure the amount of thyroid hormone
produced. The tests also measure thyroid-stimulating hormone (TSH). An
X-ray study of the thyroid (radioactive iodine scan) should not be done
during pregnancy.
With hypothyroidism, thyroid replacement
(thyroxin) is prescribed. It is believed to be safe during pregnancy.
Your healthcare provider may check the level during pregnancy with a
blood test to make sure you’re receiving enough of the hormone.
If you have hyperthyroidism, treatment is
the medication propylthiouracil. It passes through the placenta to the
baby, so ask your healthcare provider to prescribe the lowest possible
amount to reduce risk to your baby. Blood testing during pregnancy is
necessary to monitor the amount of medication needed. After delivery,
it’s important to test the baby and to watch for signs of thyroid
problems.
Iodide is another medication
used for hyperthyroidism, but it shouldn’t be used during pregnancy. It
can harm a developing baby. Pregnant women with hyperthyroidism should not be treated with radioactive iodine either.
Velocardiofacial Syndrome (VCFS)
Velocardiofacial syndrome (VCFS) is a genetic condition that may be hereditary. It is known by many names, including Shprintzen syndrome, craniofacial syndrome and conotruncal anomaly face syndrome. VCFS is one of the most common syndromes in humans, second only to Down syndrome in frequency.
The term velocardiofacial derives
from three Latin words: “velum” meaning palate, “cardia” meaning heart
and “facies,” having to do with the face. It is characterized by
various medical problems. The immune system, endocrine system and
neurological system may be involved. Symptoms do not all occur 100% of
the time. Most people with VCFS exhibit a small number of problems;
many problems are relatively minor.
The exact cause of velocardiofacial
syndrome is unknown; however investigators have identified a
chromosomal defect in people with VCFS. Most children who have been
diagnosed with this syndrome are missing a small part of chromosome 22.
If you have acid reflux, stay away from
foods that could add to the problem. Some to avoid include acid foods,
such as tomatoes and citrus fruit, and spicy and fried foods.
Only one parent must have the chromosomal
change to pass it along to a child. A parent with velocardiofacial
syndrome has a 50/50 chance of having a child with it. However, it’s
estimated VCFS is inherited in only 10 to 15% of cases. Most of the
time neither parent has the syndrome nor carries the defective gene.
The occurrence of congenital heart
disease is most often the leading factor in diagnosis. Diagnosis is
most frequently made using a genetic test called a FISH analysis (fluorescent in situ hybridization),
which is almost 100% accurate. If the test shows chromosome 22 is not
complete, the person has VCFS. If the test fails to show the deletion,
the person does not have VCFS.
Familial Mediterranean Fever (FMF)
Familial Mediterranean Fever (FMF)
occurs most often in Sephardi Jews, Armenians, Arabs and Turks. As many
as one in 200 people in these populations have the disease; 20% are
carriers. However, cases have occurred in other groups, particularly
Ashkenazi Jews. About 50% have no family history of the disorder.
FMF is inherited and usually
characterized by recurrent episodes of fever and inflammation of the
abdominal membrane (peritonitis). Less frequently, pleuritis,
arthritis, skin lesions and pericarditis can occur.
Grandma’s Remedy
If you want to avoid using medication,
try a folk remedy. If you experience leg cramps, mix together 2
teaspoons of apple-cider vinegar and 1 teaspoon of honey in a glass of
warm water, and drink it before bed.
Onset of the disease usually occurs
between the ages of 5 and 15 but may also occur during infancy or much
later. Attacks have no regular pattern of recurrence and usually last
24 to 72 hours; some last for as long as a week. High fever (as high as
104F; 40C) is usually accompanied by pain. Abdominal pain occurs in
nearly all sufferers and can vary in severity with each attack. Other
symptoms include joint pain and a rash on the lower leg. Most people
recover quickly and are OK until the next attack. Narcotics are
sometimes needed for pain relief.
Currently, no diagnostic test for FMF is
available. The problem is diagnosed more on the basis of repeated
episodes. However, researchers have identified the gene for FMF and
found several different gene mutations that can cause the disease. The
gene is found on chromosome 16. A protein assists in keeping
inflammation under control by turning off the immune response. Without
this function, an attack of FMF occurs.
Researchers continue to work to develop a
blood test to diagnose FMF. With more research, it may also become
easier to recognize environmental triggers that lead to attacks, which
may lead to new treatments for FMF.
Some Information May Scare You
If a woman experiences a serious
problem, she and her partner will probably want to know as much about
it as possible. If a woman has a friend or knows someone who has
problems during pregnancy, reading about it might relieve her fears. We
also hope our discussions can help you start a dialogue with your
doctor, if you have questions.
Nearly all pregnancies are uneventful,
and serious situations don’t arise. However, please know we have tried
to cover as many aspects of pregnancy as we possibly can so you’ll have
all the information at hand that you might need and want. Knowledge is
power, so having various facts available can help you feel more in
control of your own pregnancy. We hope reading information helps you
relax and have a great pregnancy experience.
If you find serious discussions
frighten you, don’t read them! Or if the information doesn’t apply to
your pregnancy, just skip over it. But realize information is there if
you want to know more about a particular situation.
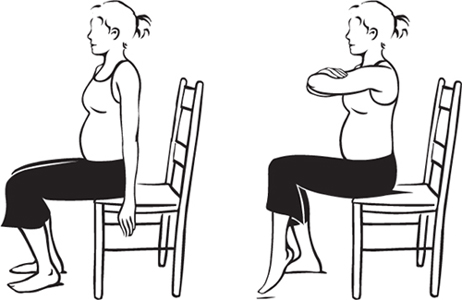
Exercise for Week 25
Sit tall at the edge of a
straight-backed side chair. Fold your arms in front of you, at shoulder
height, and slowly lean forward a bit. In this position, lift your left
foot off the floor, and hold for 5 seconds; be sure you are sitting
erect. Lower your left leg. Do 5 times for each leg. Stretches and strengthens abdominal muscles, thigh muscles and lower-back muscles.