7. You Should Also Know
MRSA
Methicillin-resistant Staphylococcus aureus (MRSA; sounds like MERSA)
is a bacteria that causes infections that are difficult to treat
because antibiotics often don’t work against them. The bacteria
(Staphylococcus aureus, also called staph) are resistant to, or develop resistance to,
many antibiotics. Bacteria have adapted or changed so antibiotics that
were effective in the past no longer work. Staph bacteria have proved
to be good at developing resistance to antibiotics.
Methicillin is a strong antibiotic that
was useful in treating staph in the past but is less useful today.
Besides methicillin, other antibiotics that are ineffective against
MRSA include dicloxacillin, nafcillin and oxacillin. A nickname used in
the media for MRSA or Staphylococcus aureus is “super-bug.”
Some experts believe staph has become
resistant because of overuse of antibiotics. Treating every cough, cold
or earache with antibiotics gives the staph bacteria an opportunity to
develop resistance. Antibiotics that do work against MRSA include vancomycin, doxycycline and TMP-SMZ (trimethoprim/sulfamethoxazole).
MRSA is a serious infection and may be
deadly. It’s passed from person to person, usually by poor hygiene. It
can start as inflamed skin, with boils or pimples. The area may be red
and hot to the touch. MRSA can spread through the bloodstream. When
this happens, it can cause sepsis or septic shock. It’s estimated that
in the United States in 2005, nearly 100,000 serious infections
involved MRSA, and about 19,000 people died.
A very common location of MRSA is the
nose or nostrils. Other possible sites are open wounds, I.V. catheters
and the urinary tract. Many hospitals and surgical centers routinely
perform a nasal culture for MRSA when a patient is admitted.
Washing your hands with regular soap,
alcohol-based foams or hand sanitizers works well in preventing MRSA.
Don’t share towels, soap or other personal items. If you have a cut or
abrasion, keep it clean, dry and covered. If you develop any pimples or
boils, don’t pop them. Keep the area tightly covered, and call your
healthcare provider immediately.
There are safe antibiotics to use during
pregnancy. Evidence doesn’t indicate MRSA during pregnancy causes
increased risk of miscarriage or birth defects. It’s very unlikely you
will pass MRSA to baby during delivery. In addition, it’s safe to
breastfeed if you have MRSA.
Pregnant women may be at greater risk for
MRSA because of decreased immunity. If either you or your partner work
in a hospital or healthcare facility, prison or
anyplace where you have a lot of contact with people, you could be at
risk. Discuss any of your concerns with your healthcare provider. He or
she can give you advice about your particular situation.
When to Call Your Healthcare Provider.
Call your healthcare provider if you believe you have been exposed to
MRSA. Take care of cuts and scratches. Know what a MRSA infection looks
like—it usually begins as a skin infection then develops small red
bumps like pimples. This can be accompanied by a fever or a rash.
Your healthcare provider can lance and
clean the infected area. Cultures or rapid tests of the skin can be
done. A vaccine against MRSA is being developed.
Grandma’s Remedy
If you want to avoid using medication,
try a folk remedy. Eat 1 teaspoon of honey before bedtime to help you
sleep. Honey helps stabilize blood sugar while it increases melatonin
levels and decreases stress hormones.
Group-B Streptococcus Infection (GBS)
Group-B streptococcus (GBS) is a type of
bacteria found in up to 40% of all pregnant women. A GBS infection
rarely causes problems in adults but can cause life-threatening
infections in newborns. GBS passed to a newborn during birth can cause
a blood infection, meningitis or pneumonia in the baby.
In women, GBS is most often found in the
vagina or rectum. It is possible to have GBS in your system and not be
sick or have any symptoms. It is recommended all women be screened for
GBS between 35 and 37 weeks of pregnancy. If tests show you have the
bacteria but no symptoms, you are colonized. If you’re colonized, you can pass GBS to your baby.
The battle to eradicate GBS is one of the
true medical success stories. Before the 1990s, 7500 newborns
contracted the infection each year; 30% of those babies died. Today,
only 1600 cases are reported each year. Much of the success has been
the result of healthcare providers following the Centers for Disease Control and Prevention (CDC) guidelines, which include the following:
• a late prenatal culture (35 to 37 weeks) for vaginal and rectal GBS colonization
• an earlier culture (earlier than 35 weeks), based on clinical risk factors
• antibiotics prescribed to all carriers—penicillin G is the antibiotic of choice, followed by ampicillin
• antibiotics prescribed for any woman who has given birth to a previous infant with proven GBS infection
If you’re allergic to ampicillin or
penicillin, clindamycin is usually given. In this case, tests to see if
clindamycin kills the GBS bacteria can be done. If these tests aren’t
available, you may receive vancomycin. In some cases, cefazolin can be
given.
The CDC, the American College of
Obstetricians and Gynecologists (ACOG) and the American Academy of
Pediatrics (AAP) have developed recommendations aimed at preventing
this infection in newborns. They recommend all women with risk factors
be treated for GBS. Risk factors include giving birth to a previous
infant with GBS infection, preterm labor, ruptured membranes for more
than 18 hours or a temperature of 100.4F (38C) immediately before or
during childbirth. In addition, if you’ve had a bladder infection with
a positive strep-B urine specimen during pregnancy, you should receive
antibiotics at delivery.
Child-Care Decisions
You may think decisions about child care
don’t need to be made for quite a while. However, it’s time to start
thinking about it if you plan to return to work after baby’s birth.
During your third trimester, you may
discover your nesting instinct—the overwhelming urge to clean and get
organized. Experts believe this may be caused by an increase in
oxytocin.
Quality care is in high demand and short supply! Experts advise you to begin looking for a child-care situation at least 6 months before you need it. For some women, that may be the end of the second trimester!
Dad Tip
Now is the time to think about changing
your work schedule so you can be near home during the last part of the
pregnancy and after baby is born. If you travel a lot, you may need to
alter your schedule. Babies come on their own schedule. If you want to
be present for the delivery, plan ahead!
Mad Cow Disease
We’ve all heard about mad cow disease,
an illness in cattle. The type that affects humans is a variant of
Creutzfeldt-Jacob disease, called vCJD. It is extremely hard to
contract vCJD; only a few cases have occurred in the United States. It
can take many years (even decades) for the disease to progress in a
human.
You can put your mind to rest about
eating beef in the United States. Our beef is tested extensively, so
you have little cause for concern. If you travel outside the country,
avoid eating beef in countries that are at risk.
Some Information May Scare You
In an effort to give you as much
information as possible about pregnancy. The
information is not included to frighten you; it’s there to provide
facts about particular medical situations that may occur during
pregnancy.
If a woman experiences a serious
problem, she and her partner will probably want to know as much about
it as possible. If a woman has a friend or knows someone who has
problems during pregnancy, reading about it might relieve her fears. We
also hope our discussions can help you start a dialogue with your
doctor, if you have questions.
Nearly all pregnancies are uneventful,
and serious situations don’t arise. However, please know we have tried
to cover as many aspects of pregnancy as we possible can so you’ll have
all the information at hand that you might need and want. Knowledge is
power, so having various facts available can help you feel more in
control of your own pregnancy. We hope reading information helps you
relax and have a great pregnancy experience.
If you find serious discussions frighten
you, don’t read them! Or if the information doesn’t apply to your
pregnancy, just skip over it. But realize information is there if you
want to know more about a particular situation.
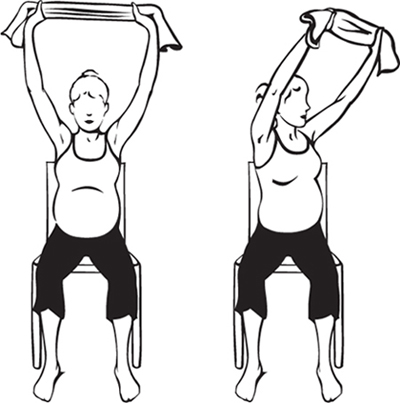
8. Exercise for Week 30
Sit tall on a straight-backed side
chair. Hold a towel above your head, with your hands shoulder-width
apart. Slowly twist from your waist to the left side as far as is
comfortable for you. Return to the center, then twist to the right. Do
8 times. Stretches spine, and strengthens shoulders and upper-back muscles.