Vaginal Birth after Cesarean (VBAC)
Should you attempt a vaginal delivery
after having had a Cesarean delivery? Medically speaking, the method of
delivery isn’t as important as the well-being of you and your baby.
Before any final decision is made, weigh the risks and benefits. In
some cases, there may not be any choice in the matter. In other cases,
you and your doctor may decide to let you labor for a while to see if
you can deliver vaginally.
Some women like having a repeat Cesarean
delivery because they don’t want to go through labor only to end up
with a Cesarean delivery. You may need another Cesarean if you have had
problems with this pregnancy. Discuss it with your doctor if you have
questions.
If you are small and the baby is large,
you may need another Cesarean. Multiple fetuses may make vaginal
delivery difficult or impossible without danger to the babies.
If a woman has a Cesarean delivery, she is at increased risk for post-partum depression.
Inducing labor with a VBAC may be
necessary; however, there’s an increased risk of the uterine scar from
an earlier Cesarean stretching and pulling apart with induction. This
is especially true if hormones are used to ripen the cervix and/or
induce labor. It is believed that contractions may be too strong for a uterus scarred by previous surgery. A repeat Cesarean may be advised to avoid rupturing the uterus.
Risk also increases for a woman who gets
pregnant within 9 months of having a previous Cesarean. In this case,
the uterus is more likely to rupture during a vaginal delivery.
Researchers believe this might occur because it can take from 6 to 9
months for the uterine scar to heal (this is the scar on the uterus—not
your abdomen). Until enough healing time has passed, the uterus may not
be strong enough to stand up to the stress of a vaginal delivery. VBACs
are safest when at least 18 months have passed between the previous
Cesarean and the attempted vaginal delivery.
Advantages of VBAC include a decreased
risk of problems associated with surgery, which a Cesarean is. Recovery
after a vaginal delivery is shorter. You can be up and about in the
hospital and at home in a much shorter amount of time.
If you want to try VBAC, discuss it with
your doctor in advance so plans can be made. Not all hospitals are
equipped for VBAC. During labor, you will probably be monitored more
closely. You may be attached to I.V.s, in case a Cesarean delivery
becomes necessary.
Consider the benefits and risks in
deciding whether to attempt a vaginal delivery after a previous
Cesarean delivery. Discuss them at length with your doctor and your
partner before making a final decision. Don’t be afraid to ask your
doctor his or her opinion of your chances for a successful vaginal
delivery. He or she knows your health and pregnancy history.
Tip for Week 37
Be prepared for delivery with bags packed, insurance papers filled out and available, and other important details taken care of.
6. Your Nutrition
You and your partner have been invited to
a big party. You’ve been careful about your nutrition, and your
pregnancy is almost over. Should you let yourself go, and eat and drink
whatever you want? Probably not. Maintain your good eating habits. You can
party healthfully. Before you go, eat or drink something to take the
edge off your appetite. It may be easier to avoid high-fat,
high-calorie foods if you’re not ravenous.
At the party, eat food when it’s fresh or
hot—at the beginning of the party. As the party goes on, the food may
not be chilled or heated enough to prevent bacteria from growing. So
eat early or when dishes are refilled.
Avoid alcohol. Drink fruit juice “spiked”
with ginger ale or lemon-lime soda. If it’s the holiday season and
they’re serving eggnog, have a glass if it’s pasteurized and
alcohol-free.
Raw fruits and vegetables can be
satisfying. Avoid raw seafood, raw meat and soft cheeses, such as Brie,
Camembert and feta. They may contain listeriosis.
Stay away from the refreshment
table if you can’t resist the goodies. It may feel better to sit down
(away from food), relax and talk with friends.
Will You Have an Enema?
Will you be required to have an enema when you arrive at labor and delivery? An enema
is a procedure in which fluid is injected into the rectum to clear out
the bowel. An enema before labor can make the birth of your baby more
pleasant for you. When the baby’s head comes out through the birth
canal, anything in the rectum also comes out. An enema decreases the
amount of contamination from feces during labor and at the time of
delivery, which may also help prevent infection.
Dad Tip
You may not understand how nervous your
partner may be about getting in touch with you when she needs you. Be
sure to let her know how she can reach you at work or when you’re out.
Keep your cell phone or a beeper with you all the time. This can
comfort her and provide her with peace of mind.
Most hospitals offer an enema at the
beginning of labor, but it’s not always mandatory. There are certain
advantages to having one early in labor. You may not want to have a
bowel movement soon after your baby’s birth because of discomfort. Having an enema before labor can prevent this discomfort.
Ask your doctor if an enema is routine or
considered helpful. Tell him or her you’d like to know about the
benefits of an enema and the reasons for giving one. It isn’t required
by all doctors or all hospitals.
What Is Back Labor?
Some women experience back labor. Back labor
refers to a baby coming through the birth canal looking straight up.
With this type of labor, you will probably experience lower-back pain.
Back labor can also last longer.
The mechanics of labor work
better if baby is looking down at the ground so it can extend its head
as it comes out through the birth canal. If the baby can’t extend its
head, its chin points toward its chest, which may cause pain in your
lower back during labor. Your doctor may need to rotate the baby so it
comes out looking down at the ground rather than up at the sky.
Will Your Doctor Use a Vacuum Extractor or Forceps?
The goal with every birth is to deliver
a baby as safely as possible. Sometimes baby needs a little help. Your
doctor may use a vacuum extractor or forceps to help safely deliver
baby. Vacuum and forceps delivery methods each have about the same
risks. Use of either is associated with a more frequent need for
mechanical ventilation in infants and with more 3rd- and 4th-degree perineal tears.
Vacuum extractors are used more today
than forceps. There are several types of vacuum extractors. Some have a
plastic cup that fits on baby’s head by suction. Another type has a
metal cup that fits on baby’s head. The doctor attaches the cup to
baby’s head and gently pulls on it to deliver baby’s head and body.
Forceps is a metal instrument used to
deliver babies; it looks like two large metal hands. Use of forceps has
decreased in recent years. If a lot of traction with forceps is needed
to deliver baby, a Cesarean may be a better choice. Cesarean deliveries are also used more often to deliver a baby that is high up in the pelvis.
If the possible use of a vacuum extractor
or forceps causes you concern, discuss it with your healthcare
provider. It’s important to discuss issues that may come up during
labor and delivery so you can communicate your concerns.
7. Exercise for Week 37
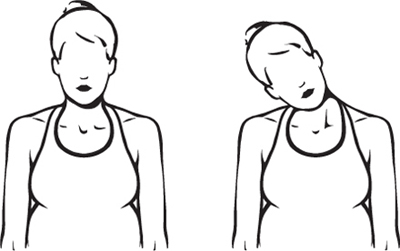
Sit on a chair or on the floor in a
crossed-leg position. Inhale, and slowly tilt your head to the right
until you feel a stretch in your neck. Breathe deeply 3 times while
holding the stretch. Slowly bring your head to the center, then tilt
your head to the left. Hold while you breathe deeply 3 times. Do 4
times on each side. Helps stretch the neck, and relieves neck and shoulder tension.