From the gut
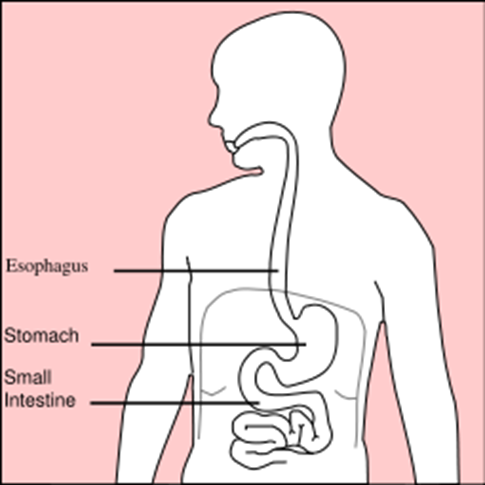
In a
surprise finding, cells in mouse intestines started producing insulin after
researchers turned off a gene. This unexpected result has the potential to
someday spur the development of new treatments for type 1 diabetes. The gut
cells began to act like insulin-producing pancreatic cells when researchers
blocked the Foxo1 gene, which controls the maturation of stem cells into adult
cells. The cells deprived of Foxo1 produced enough insulin to nearly normalize
blood glucose levels in diabetic mice. The researchers say these findings
suggest that medications targeting Foxo1 genes could turn the guts of people
with type 1 into insulin factories, though Foxo1 studies in people are still
far off.
The gut cells began to act like
insulin-producing pancreatic cells when researchers blocked the Foxo1 gene,
which controls the maturation of stem cells into adult cells.
A costly prescription
Some
doctors don’t follow expert advice on how to treat people with newly diagnosed
type2 diabetes, a study found. The American Diabetes Association generally
recommends using metformin first, along with lifestyle changes. Researchers
analyzed a mountain of data from pharmacies and discovered that a third of
people with 2 don’t start with metformin. While 18 percent initiated treatment
with a sulfonylurea, also a time-tested and inexpensive type2 medication, 1 in
5 people was prescribed newer and far more expensive medications, including thiazolidinediones (glitazones)
and DPP-4 inhibitors. Insurers and patients together paid an average of $677
over six months for these medications while metformin cost just $116. The
researchers acknowledge that in some cases metformin isn’t a good choice, such
as for people with kidney disease or heart failure.

Some doctors don’t follow expert advice on how
to treat people with newly diagnosed type2 diabetes
Pregnancy under pressure
Women with
high blood pressure (hypertension) during pregnancy are at risk of developing
type2 diabetes later on, a study found. Researchers looked at the medical
records of almost 6,000 women; those who’d had hypertension during pregnancy
were five times more likely to develop type 2 diabetes over the next eight
years than those without high blood pressure. The risk rose even higher for
women who were obese or had high LDL (“bad”) cholesterol. Researchers say that
doctors should target women who develop hypertension during pregnancy for
diabetes prevention.

Women with high blood pressure during pregnancy
are at risk of developing type2 diabetes later on
Formula and type 1
Is the
bovine insulin in cow’s milk formula a trigger for type 1 diabetes? Babies at
genetic risk for type 1 diabetes who drank cow’s milk formula during the first
six months of life (when breast milk was unavailable) appeared, at age 3, to be
more likely to go on to develop the disease than those weaned on an
insulin-free formula, a Finnish study found. Researchers hypothesized that cow
insulin could trigger the infant immune system to misfire, paving the road to
type 1 diabetes. They did blood tests to detect autoantibodies – markers of a
dysfunctional immune system – and found fewer autoantibodies in the children on
insulin-free formula.

Cow’s milk
Promising type 2 drug
A novel
drug successfully lowered blood glucose levels in people with type 2 diabetes,
researchers reported, without increasing the risk for low blood glucose
(hypoglycemia). People taking the experimental drug TAK-875
once daily for three months lowered their A1Cs (average blood glucose over the previous two to three months) an
average of 1.1 percentage points. TAK-875 activates a protein called the free fatty
acid receptor that is found in the pancreas.
When it interacts
with fats in the body, the protein can trigger the release of insulin, but only
if glucose levels are rising. This glucose dependence helps TAK-875 control
blood glucose without causing hypoglycemia, the researchers say. Longer and
larger studies are needed to determine whether the drug is safe and effective.