Right now (Con’t)
Enlist
food favorites.
After dosing rapid-acting insulin, it’s
important to eat some food containing carbohydrate, but fussy eaters may
refuse. Rose’s solution: Find a food item with the number of carbs your child
is supposed to eat per meal, and make sure you have it at the ready. When her
daughter Adalyne turned her nose yp at lunch or dinner, Rose would whip up a
serving of oatmeal with about 30 grams of crabs.

Enlist
food favorites
Set your
alarm.
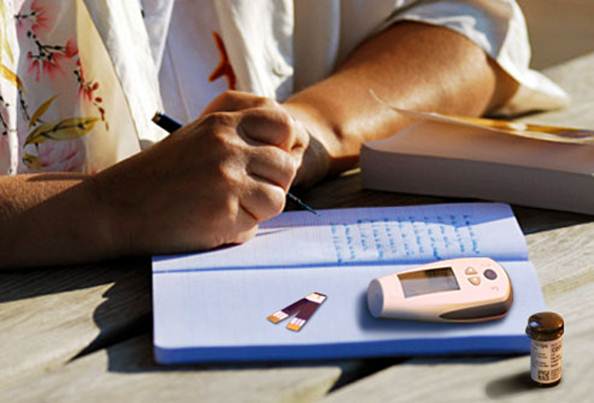
Prepare to check yout child’s blood glucose
during the middle of the night (2 to 3 a.m.) as you adjust overnight insulin,
to catch or prevent any hypoglycemic episodes and to log patterns. Overnight
checks are also important if your child is ill ot physically active in the
afternoon or evening. While there’s nothing you can do to prevent exhaustion
from those interrupted nights, there are steps you can take to make the process
easier. For starters,buy a headlamp, says Rose. It left her hands free for
testing her daughter’s blood glucose in the dark.
Prepare
to check yout child’s blood glucose during the middle of the night (2 to 3
a.m.)
Many children, including those of the parents
interviewed for this article, sleep right through nighttime checks. You will
have to wake them, however, if their blood glucose dips too low. In that case,
it helps to have a quickly digested source of glucose, such as glucose gel or
juice, nearby.
Check blood ketones. On sick days (even with
normal or only slightly elevated glucose levels) or when blood glucose gets too
high – usually over 250 mg/dl – you’ll need to check your child for ketones.
They are waste products that build up when there’s not enough insulin available
in the body. Left unchecked, high levels of ketones can lead to diabetes
ketoacidosis and even death. Most people with type 1 diabetes check ketones
using a simple urine test, but the process is a bit more difficult for babies
and toddlers who haven’t been potty trained. Talk with your provider about
blood ketone tests that work similarly to blood glucose meters. But keep in
mind, they’re less commonly prescribed than urine ketone test kits and may not
be covered under your insurance.
Very
soon
Inject with less pain. Most diabetes experts
will tell you that needles today are tiny, and that’s true – they’re shrunk
considerably since the advent of insulin. But that
doesn’t mean shots are always painless. That said, there are steps you can take
to make an insulin injection inflict as little pain as possible. Many parents
rely on ice for injections. Numbing gel (available over the counter or by
prescription) is a good option for insulin pump infusion set insertions, but it
can take up to an hour to work.

Are
you using room-temperature insulin?
If your child is complaining about the pain
of an injection, first consider your technique. Are you using room-temperature
insulin? Injections hurt more when insulin is cold. Open vials or pens at room
temperature can be used for 30 days. Cold insulin will also result in more air
bubbles, increasing pain. (And you lose insulin to the air bubbles, a
significant amount when it comes to child-sized doses.) Are you quickly poking
the needle through the skin and keeping the barrel steady? When the tip of the
needle rests on top of the skin, the nerves become irritated and pain is
magnified.
The type of insulins you use may matter,
too. Insulin glargine (Lantus) has a tendency to sting because of the
preservatives in it. If it’s causing your child enough of a problem, talk with
your endocrinologist, says Maahs, because he or she may prescribe insulin
detemir (Levemir) instead.
Let
‘em play.
Gee encourages the kids she works with to
participate in what she calls medical play. If your hospital doesn’t offer the
activity, guide your kids through it at home by teaching them to give mock
blood glucose tests and insulin injections (just make sure the syringe is empty
and the needle is removed) to their stuffed animals. Even using a lancing
device on a doll or toy can help kids see there’s nothing to fear.
Get
rid of the guilt.
True, a diabetes diagnosis requires you
cram a semester’s worth of knowledge into just a few days, but for most
parents, studying up on the how-tos of diabetes management isn’t the biggest
source of stress. That’s reserved for feeling guilty about testing their little
one’s blood glucose and giving insulin injections. “When you’re pricking her
finger, she just doesn’t understand,” says Red Maxwell, whose daughter Cassie,
now 16, was diagnosed with type1 diabetes at 18 months old. “That can be really
traumatizing for a parent because you’re hurting your child – the opposite of
your instincts.”

Get
rid of the guilt
The key to shaking off the guilt, says Gee,
is to change the way you view testing and injections. “In the first two weeks,”
says Rose, “[my daughter] was very resistant to it, and it often took two of us
to check her blood sugar, one of us to restrain her and one of us to test her.
I had to separate it in my mind that every shot I was giving her was prolonging
her life.”