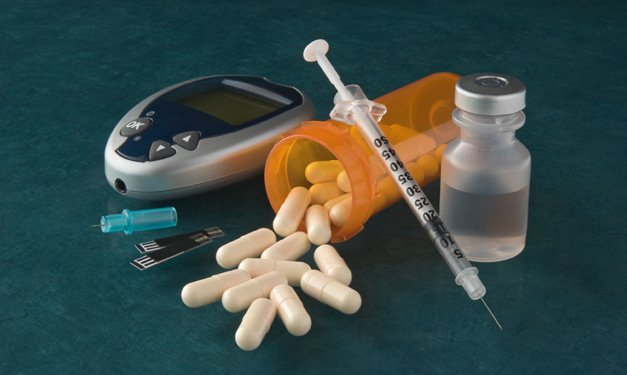
A class of injectable type 2 meds gains ground
For decades, insulin was the only injectable
diabetes medication. But in the past seven years, several
more have come on the market, including three incretin mimetics: exenatide
(Byette), long-acting exenatide (Bydureon), and liraglutide (Victoza). These
medications are approved only for the treatment of type 2 diabetes, though they
may someday be used by people with type 1 as well.

For
decades, insulin was the only injectable disbetes medication
Many have heralded this class of medications
as a monumental advance in diabetes care, and indeed their attractive
characterstics include promoting weight loss and carrying a low risk foe hypoglycemia
(low blood glucose). Here’s the skinny on incretin mimetics: how they work, how
they differ, and what to consider discussing with your doctor.
Inner workings
Incretins are a group of hormones, and all
three U.S.-approved incretin mimetics mimic the same incretin hormone,
GLP-1. This hormone is made by specialized cells in the small intestine, which
release the incretin into the body when sense food from a meal passing through
the intestines.
This
hormone is made by specialized cells in the small intestine
Once in the bloodstream, incretins travel
around the body, affecting several organs, including the pancreas. Incretins
spur cells in the pancreas to make more insulin in response to a rise in blood
glucose. The insulin brings blood glucose levels back down after eating.
Incretins also suppress the production of glucagon, a hormone that signals the
liver to release its glucose stores into the blood. When the liver holds back
its stored glucose, blood glucose levels are more likely to remain in the normal
range. “Glucagon suppression may account for 50 percent of the incretin
effect.” Says Carol Wysham, MD, clinical associate professor of medicine at the
University of Washington School of Medicine.
People with type 2 diabetes have depressed
GLP-1 levels. However, GLP-1 itself would make a poor drug because it is
quickly broken down in the body by an enzyme called DPP-4. (DPP-4 inhibitors
are another class of type 2 medications; they increase GLP-1 levels by slowing
the enzyme’s effects). A breakthrough came when researcherers discovered a
protein in the saliva of the Gila monster, a Southwestern lizard. The protein,
exenatide, looks similar to GLP-1 and works about the same, but it goes
unrecognized by DPP-4. Later, protein engineers developed liraglutide by
employing a subtle chemical trick that changes GLP-1 just a tiny bit, but
enough to fool DPP-4. Because they are small proteins, incretin mimetics be
injected so that they enter the bloodstream. If the proteins were taken orally,
gastric juices would digest them.
When doctors talk about incretin mimetics,
weight loss invariably comes up early in the conversation. “No other type 2
drug on the market results in [so much] weight loss,” says Filip Knop, MD, PhD,
head of the Diabetes Research Divison at the University of Copenhagen. But
results vary, and some people will lose little or no weight. Another bonus is
that incretin mimetics aren’t likely to cause hypoglycemia. “they only exert
their effects when glucose is relatively high,” says Knop. “When glucose is
low, they have no effect on insulin secretion.”
Same difference
The three incretin mimetics differ in how
often they’re taken. Exenatide needs to be injected twice a day, in the hour
before a meal. Liraglutide is taken once daily, at any time and independent of
meals. Long-acting exenatide is a week’s worth of regular exenatide that is
designed to release gradually. It is injected every seven days, at any time of
day, with or without meals.

All
the incretin mimetics sometimes cause discomfort
All the incretin mimetics sometimes cause
discomfort. Gastrointestinal side effects, such as nausea, vomiting, and
diarrhea, are not uncommon complaints. Many people experience mild nausea at
first, which goes away with time, and slowly work up to taking a full dose as
directed. Some of the medications may be tolerated better than others. “A
general rule,” according to Wysham, “is that the longer the medicaiton works,
the less severe the side effects.” Accordingly, once-weekly exenatide use is
associated with the least stomach distress.
Researchers are also comparing the incretin
mimetics’ results in lowering blood glucose and promoting weight loss. So far,
they have found greater differences in A1C reduction (average blood glucose
over the previous two to three months) than in weight loss.
A difference between exenatide and liraglutide
is in how the body metabolizes the medications. Liraglutide is eventually
broken down by enzymes in the body, while exenatide is excreted through the
kidneys, which makes it unsuitable for people with kidney problems.
Other considerations
One of the biggest drawbacks of incretin
mimetics is their cost. “The prices are extraordinarily hard to swallow,” says
Wysham, ranging from around $300 a month for exenatide to over $400 for liraglutide.
Incretin mimedics may not be covered as well by insurance plans as other
diabetes medications. “The major barrier from my perspective is that my
patients are willing, but insurers are not,” says Wysham.
Another concern is that because these drugs are
relatively new, there may yet be safety issues. All incretin mimetics carry a
black box warning about thyroid cancer. Stuides in rats showed that the drugs
did increse the likelihood the animals would get thyroid cancer; the effects in
humans are uncertain at this time. There have also been reporst of people
developing pancreatitis after starting an incretin mimetic. “As doctors, we
need to inform patients on these risks,” says Knop, “but the data are not the
best. For now, it’s just a signal that we have to take seriously, but the exact
connection is not well established.”
Incretin Mimetics and Type 1
Diabates
Care
Some research ahs hinted that incretin
mimetics may actually give the insulin-producing beta in the pancreas a boost.
This opens the door to the possibility that those with type 1 might benefit
from the drugs, as an add-on to insulin. A small July 2011 study, published in
Diabates Care, found that liraglutide treatment in poeple with type 1 lowered
blood glucose levels and reduced insulin doses. The researchers said that
participants’ beta cell function appeared to improve, too. Filip Knop, MD, PhD,
of the University of Copenhagen says that in an ongoing study in Denmark,
liraglutide is being given to people with newly diagnosed type 1, who still
maintain some beta sell function. Researchers are “hoping they can prevent the
immune system from killing those beta cells by helping the beta cells preserve
themselves,” he says.