Diet and exercise can help
A GDM diagnosis can serve as an early warning,
motivating at-risk women to make permanent lifestyle changes. “Even if
treatment only delays diabetes by 10 or 15 years, that’s huge,” Metzger says.
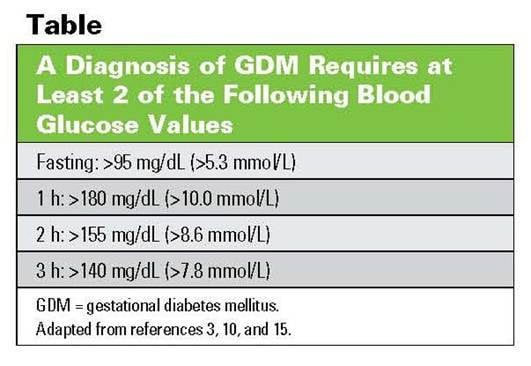
GDM
diagnosis
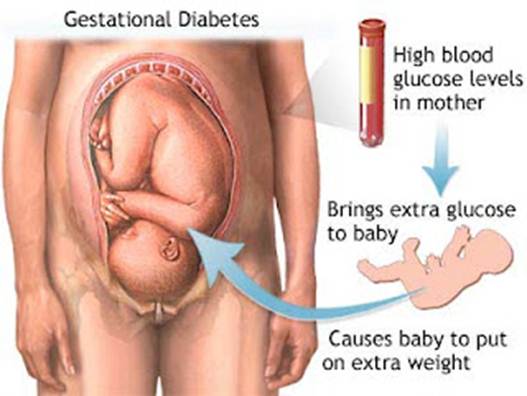
Hillier found the risks to children were
reduced when women with GDM were treated with diet changes, such as eating
fewer sweets and starchy foods, smaller, more frequent meals and more fruits
and vegetables; increased exercise; and, if that was insufficient, by adding
medication, typically insulin. When women remained untreated, their baby’s
risk of being overweight or obese at ages 5 to 7 was nearly twice as high. “But
the children of women who were treated for GDM had no greater risk of obesity
or being overweight compared with children of mothers who had normal blood
sugar during pregnancy,” Hillier says. “This suggests that treating moms during
pregnancy gives their babies a fighting chance for a normal metabolism.”
Like Paetsch, Jennie Wolter, 32, was
shocked by a GDM diagnosis because she, too, had no obvious risk factors. “But
I came to terms with it when I was assured by my health care providers that I
could manage the risks and have a healthy baby,” says Wolter, the community
relations manager for a nonprofit organization in Sacramento, Calif. In
addition to changing her diet with the help of her midwife, a nutritionist, a
nurse and a supervising OB, Wolter also credits exercise with helping her
avoid having to take insulin. “My team told me that blood sugar could be well
controlled by getting some exercise after each meal,” she says. When Wolter
delivered her 8-pound, 6-ounce baby vaginally, she was only 15 pounds over her
pre-pregnancy weight—with her caregivers’ blessing.
Diagnosis
of diabetes during pregnancy
Paetsch did need to take insulin during her
pregnancy, and she credits her diet and exercise changes for feeling better
physically at that point than she had in a long time, for weighing about 10 to
12 pounds less today than when she became pregnant and for teaching her a
healthier way to live, long-term. “Monitoring my diet was a huge pain at the
time, but I learned a lot about how much self-restraint I could actually have,”
she says. She also learned she could fit in small amounts of exercise
throughout the day and have it count, the way experts say it will. “GDM felt
like such a devastating diagnosis at the time,” Paetsch says, “but it was
actually a bit of a blessing in disguise.”
Life after gestational diabetes
“To date, no intervention has been proven
to prevent gestational diabetes [GDM],” says Mark Landon, M.D., chairman of the
department of obstetrics and gynecology at The Ohio State University College
of Medicine. “However, there is evidence that diet, exercise and medication
can help women with a history of gestational diabetes avoid developing
diabetes postpartum.”

Pregnant woman in kitchen eating a salad
Breastfeeding may help as well. A 2012
study published in Diabetes Care found that women who’d had GDM and were
exclusively or mostly breastfeeding at six to nine weeks postpartum had
improved fasting blood glucose levels compared with women who were mostly or
exclusively formula- feeding their babies. More research is needed to determine
if the benefits are long-lasting, Landon says.
Nursing may also help their children.
Researchers reporting this year in the International Journal Of Obesity
studied children from birth to age whose mothers had any type of diabetes and
found that those who’d gotten at least six months of mother’s milk had
significantly lower BMIs, smaller waists and less body fat than the offspring
of diabetic mothers who breastfed less.