Getting patients and doctors to change
their approach to cancer screening is hard. But a number of organizations are
working on the problem
For example, in an initiative called
Choosing Wisely, we are working with more than two dozen medical organizations
to identify overused interventions, including screening tests such as Pap
smears for women younger than 21. Other organizations, such as the Informed
Medical Decisions Foundation, have developed brochures and videos in plain
language to help patients navigate complex medical choices. And the U.S.
Preventive Services Task Force and other groups are working to provide more
nuanced, accurate information on cancer screening tests.

Getting
patients and doctors to change their approach to cancer screening is hard
“Cancer turns out to be a much more
complicated and unpredictable disease than we used to think,” says Virginia
Moyer of the task force. “And the tests we have available to us don’t work as
well as we’d hoped, and can even cause harm.
“Scientific evidence shows that some
cancer-screening tests work, and people should focus on those tests rather than
on screening tests that are only supported by theories and wishful thinking.”
Doctor knows best?
When it comes to cancer screening, most
people do what their doctor recommends. Unfortunately, health care providers
don’t always agree on which tests are necessary. In fact, research suggests
that advice often varies among medical practices.
Although health care providers really
publish information on the percentage of their patients who are screened for
specific cancers, we were able to get that information from organizations in
Massachusetts, Minnesota, and Wisconsin. Because of differences in the data
collected from each organization, we can’t compare results. But the numbers
illustrate the variation within states, as shown below for colon-cancer
screening.
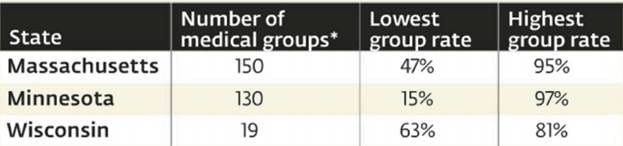
Percentage
of patients offered colon-cancer screening
(*: A medical group is one or more medical
clinics that operate as a single business.)
Bottom
line.
Don’t assume that your doctor will bring up
cancer screening or follow guidelines. So educate yourself using our Ratings as
a starting point. If you live in one of the states shown below, you can see how
practices compare on the organizations’ websites: for Massachusetts, mhqp.org;
Minnesota, mnhealthscores.org; Wisconsin, wchq.org.
Three tests to get – and eight to avoid
Screening tests for cervical, colon, and
breast cancers are the most effective tests available, according to our first
Ratings of cancer screening tests. But most people shouldn’t waste their time
on screenings for bladder, lung, oral, ovarian, prostate, pancreatic, skin, and
testicular cancers.
Notes that our recommendations often differ
with age. For example, colon-cancer screening gets our highest Rating for
people age 50 to 75 but our lowest Rating for those 49 and younger, because the
cancer is uncommon among younger people.
In addition, the Ratings are for people who
are not at high risk; those who are at increased risk, as well as those who
have signs or symptoms of cancer, may need the test or should be tested sooner
or more often.
Our Ratings are based mainly on reviews
from the U.S. Preventive Services Task Force, and independent group supported
by the Department of Health and Human Services. We also considered other
factors: evidence that emerged after the task force’s report; the number of
people affected by the cancer; the cost of testing and treatment; and the
benefits of a test beyond its ability to detect cancer.
Do the benefits of the test outweigh the harms?
|
Very likely
|
5/5
|
|
Likely
|
4/5
|
|
Normal
|
3/5
|
|
Unlikely
|
2/5
|
|
Very Unlikely
|
1/5
|
Get these screenings
Cervical
cancer

Women
age 21 to 30 should have a Pap smear every three years. Those 30 to 65 can go
fice years between Pap smears if they have had HPV testing.
5/5 for women age 21 to 65
1/5 for women of all other ages
A pap smear (a
microscopic analysis of cervical tissue samples) and a human papillomavirus
(HPV) test, which looks for the virus that can cause the cancer
Women age 21 to 30 should have a Pap smear
every three years. Those 30 to 65 can go fice years between Pap smears if they
have had HPV testing. High-risk women may need to be screened more often women
65 and older don’t need to be tested as long as they’ve had regular screenings
when they were younger. Women under 21 don’t need to be screened because the
cancer is uncommon before then and the tests are not accurate for them.
A family history of the disease, a history
of HPV infection, using birth-control pills for five or more years, having
three or more children, and having weakened immunity because of HIV infection
or other causes.
Colon cancer

People
age 50 to 75 should be regularly screened.
5/5 for people age 50 to 75
3/5 for people 76 to 85
2/5 for people 86 and older
1/5 for people 49 and younger
Colonoscopy (exam of the entire colon with
a flexible scope) every 10 years, sigmoidoscopy (exam of the lower third of the
colon) every five years plus a stool test every three years, or a stool test
every year.
People age 50 to 75 should be regularly
screened. Older people should talk with their doctor about the benefits and
harms of the test based on their health and risk factors. Younger people should
consider testing only if they are at high risk, because the cancer is uncommon
before age 50.
A family history of the disease or a
personal history of precancerous polyps, inflammatory bowel disease, obesity,
smoking, type 2 diabetes, excessive alcohol consumption, and a diet high in red
or processed meats.
Breast cancer

Women
age 50 to 75 should have mammograms every two years
4/5 for women age 50 to 74
3/5 for women 40 to 49
2/5 for women 75 and older
1/5 for women 39 and younger
Mammogram (an X-ray of the breast)
Women age 50 to 75 should have mammograms
every two years. Women in their 40s or those 75 and older should talk with
their doctor to see whether the benefits outweigh the harm based on their risk
factors women younger than 40 should consider testing only if they are at high
risk, because the cancer is uncommon at that age
A personal or family history of the cancer,
a personal history of benign breast conditions such as atypical hyperplasia,
dense breasts, menstrual periods before age 12 or after age 55, not having a child
before age 30, postmenopausal hormone-replacement therapy, obesity, excessive
alcohol consumption, smoking, or genetic susceptibility.